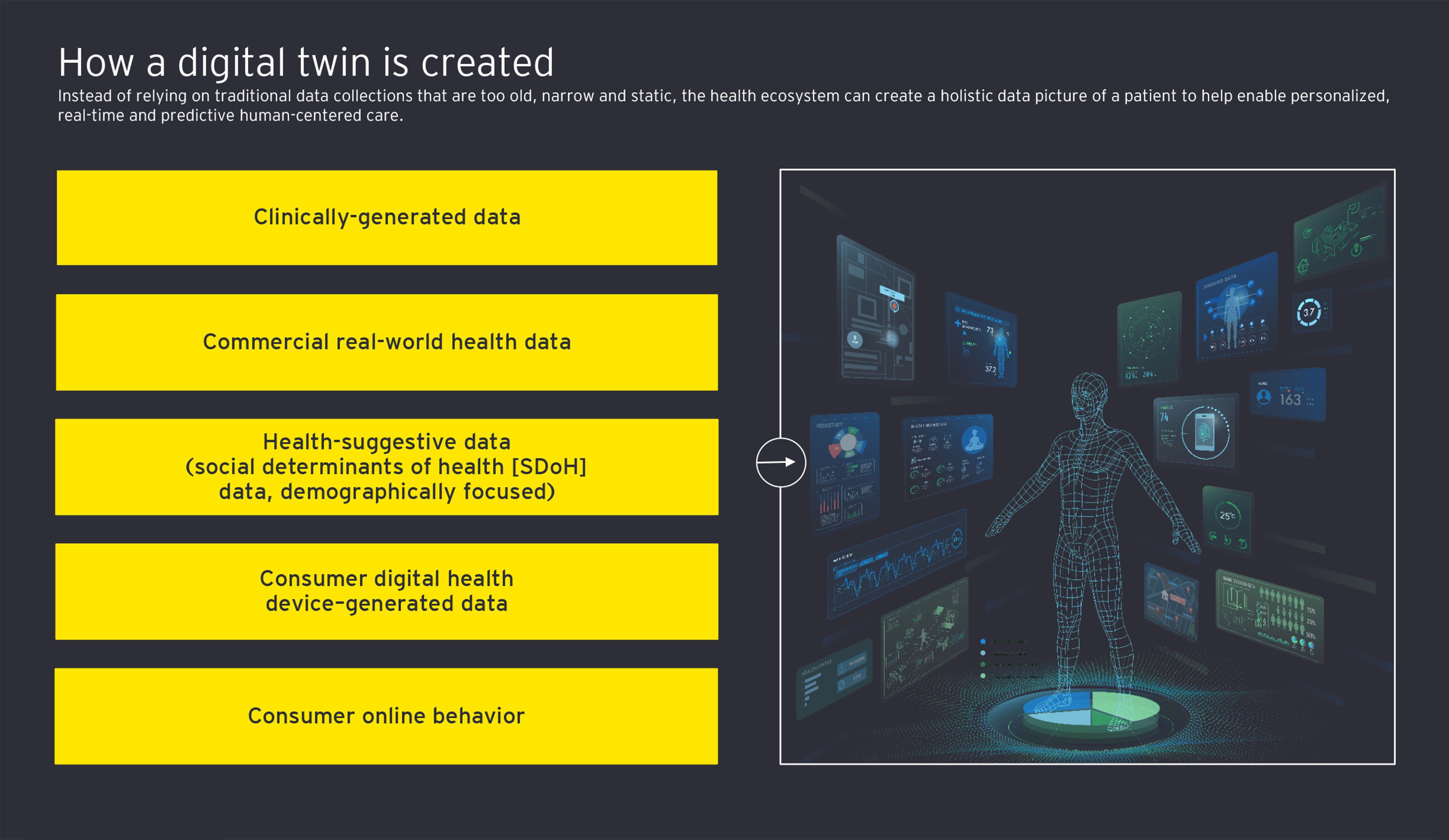
Wearable sensors can be integrated with the digital twins to produce live data streams that alert clinical teams, caregivers and the patient when action needs to be taken both inside the hospital and at home, enabling more exception-based care management. US-based BioIntelliSense has introduced the BioButton®, a medical-grade wearable sensor that captures patient vital signs and feeds the data streams to their care team, enabling clinicians to identify when new symptoms are developing or the patient needs an intervention.1
While digital twins give clinical staff a more holistic vision, they also can present an avenue to educate the patient and their caregivers about the potential medications, procedures and quality of life they face.
All of this hinges on health systems’ abilities to properly secure patient data not only to meet regulatory requirements but also to earn the trust of patients to use their data. Platforms that can unite data will require strong cybersecurity programs.
Personalized care pathways can make health systems more effective and efficient
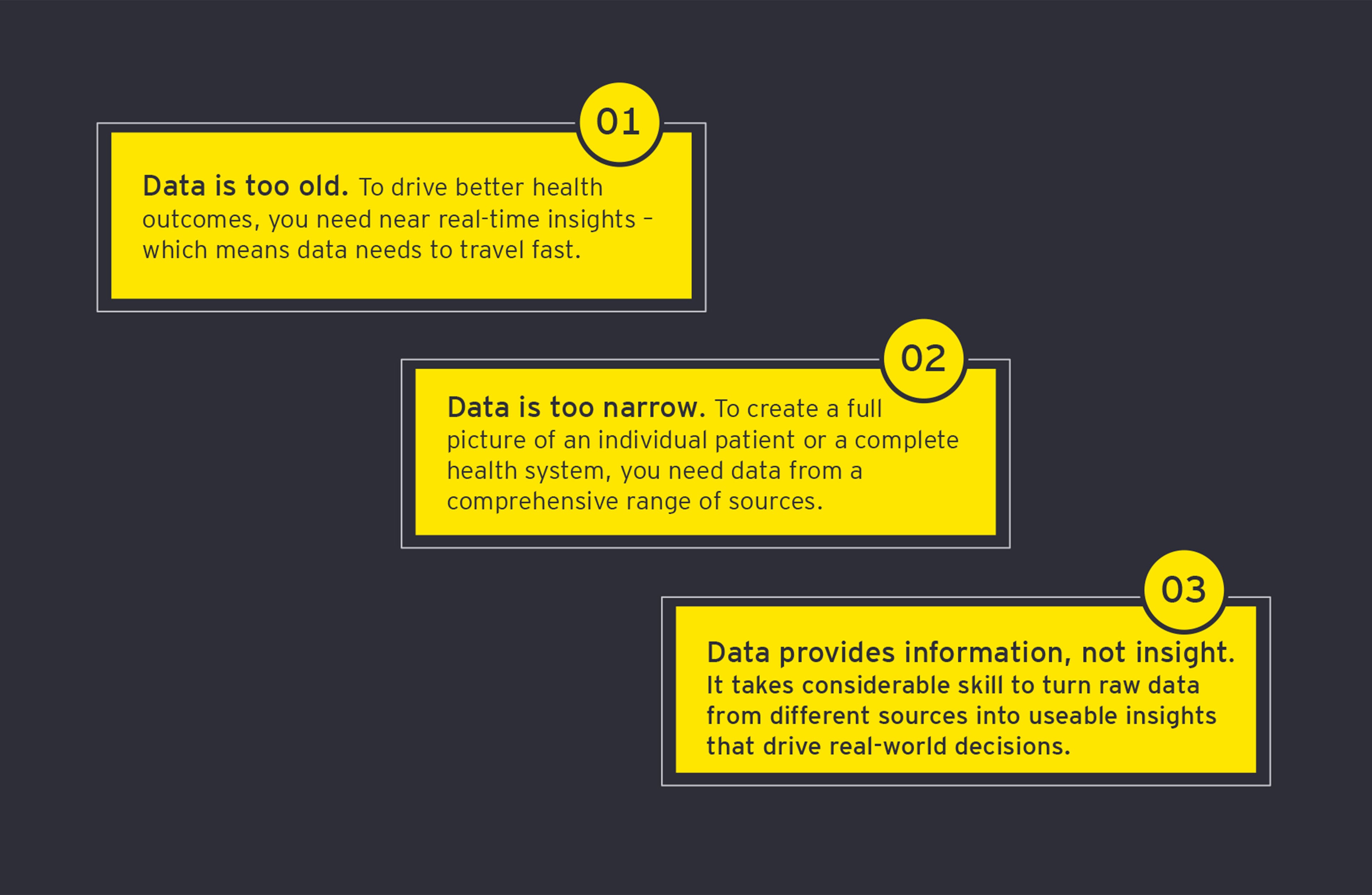
Digital twin technology presents opportunities for significant cost savings for health systems, and for payers, that are looking for providers to show value for the US$8.8 trillion that is spent globally each year on health care.2 In the US alone, the pressure is building, as the percentage of GDP devoted to health is expected to rise from 17.7% in 2018 to 19.7% by 2028.3
Routing patients to the right care is crucial for the move to value-based care to make sure the right resources are applied to each patient. A recent analysis of 27 million emergency room visits in the US showed that two-thirds were avoidable, as the conditions could be treated in primary care settings.4
For example, individuals with diabetes who do not manage their diabetes often end up developing complications, such as ulcers, heart attacks and acute kidney failure. The average cost for a patient visit to the ER for kidney disease is US$1,722, and if that patient needs to be admitted, the average cost for an inpatient stay for those with kidney disease is US$17,483.5 In 2021, 10.5% of adults across the globe had diabetes.6
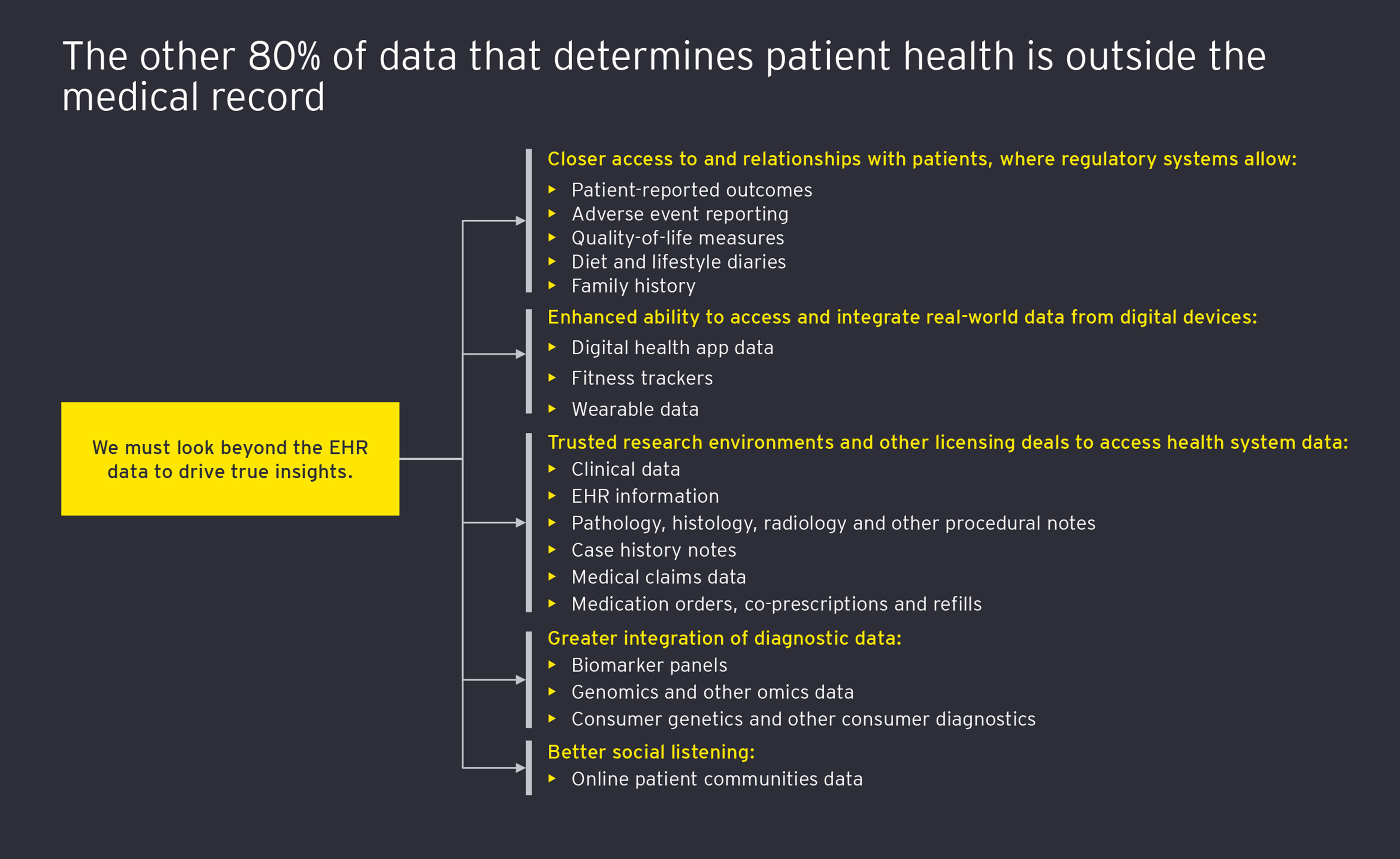
But if providers can get to the root cause of the patient not being able to manage the disease, they can help keep that patient’s health from progressing to an expensive and painful crisis. Often, the answer may be found outside the EHR, in nonmedical data sets that present a picture of the challenges the person faces in leading a healthy lifestyle.
Insights from digital twin technology can help address health inequities
As the pandemic brought to the forefront the racial and social inequities that persist in health care, health systems have an opportunity to use digital twin technology and predictive analytics on a population level to identify barriers to care and help balance outcomes.
By stratifying the risk for different segments of the population, providers as well as payers can create digital community twins that help enable them to identify vulnerable populations and develop different tracts of outreach that reflect the community needs. Where and how patients live contribute tremendously to health, as shown by asthma patients who have flare-ups from heavy smog or by individuals with chronic obstructive pulmonary disease (COPD) who repeatedly turn up in urgent care because their homes are cold and wet.
While digital patient twins may seem futuristic to an industry that may still have paper-based records or siloed data collections, the reality is that if health systems are to address the building pressure of unsustainable health care budgets, personalizing care so patients are directed to the right care at the right time and avoiding waste can be a key component. Individualized care paths can help patients avert expensive and stressful medical procedures, payers find the value they seek, and providers achieve their goal of bringing more wellness to the communities they serve.