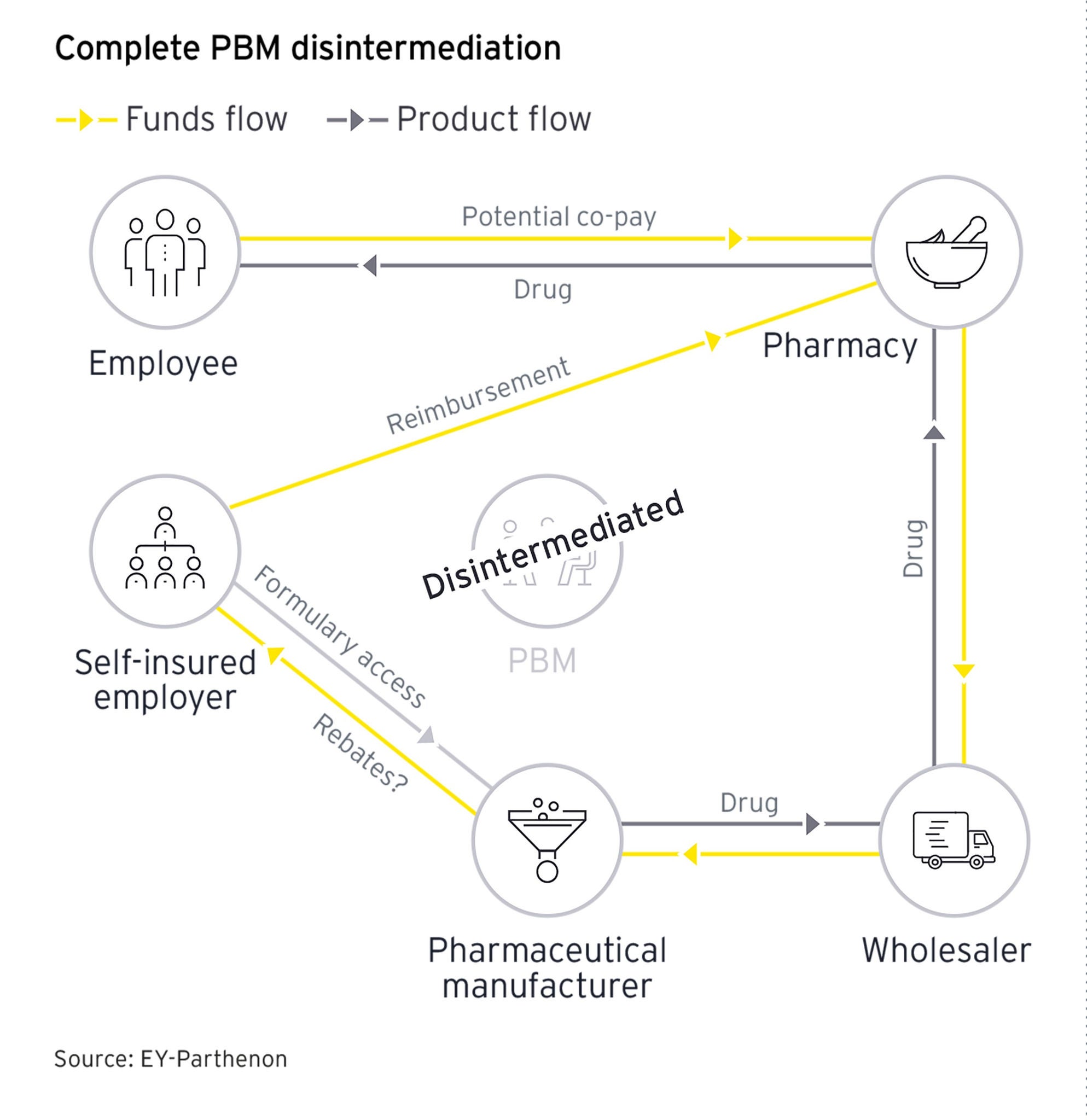
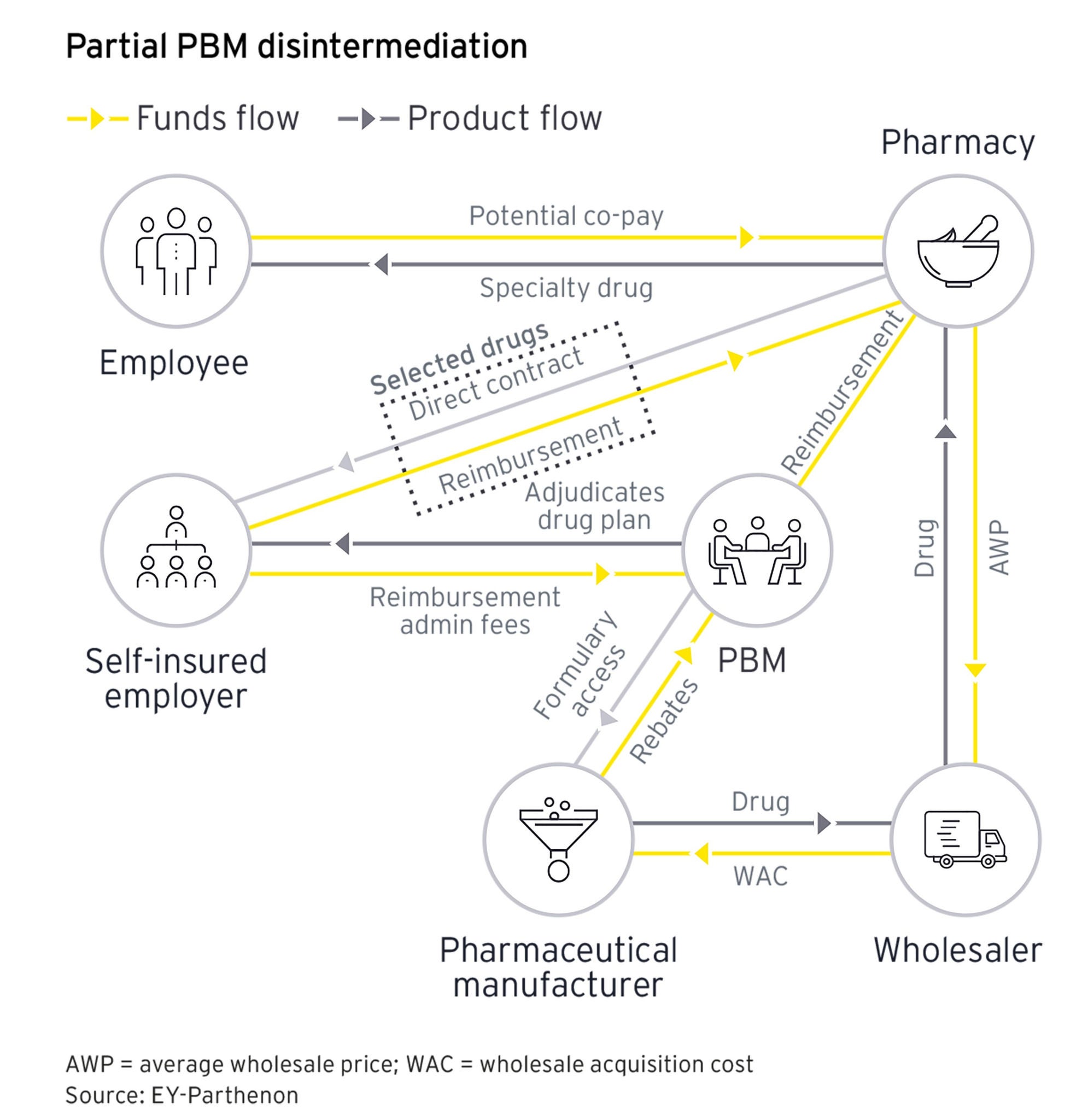
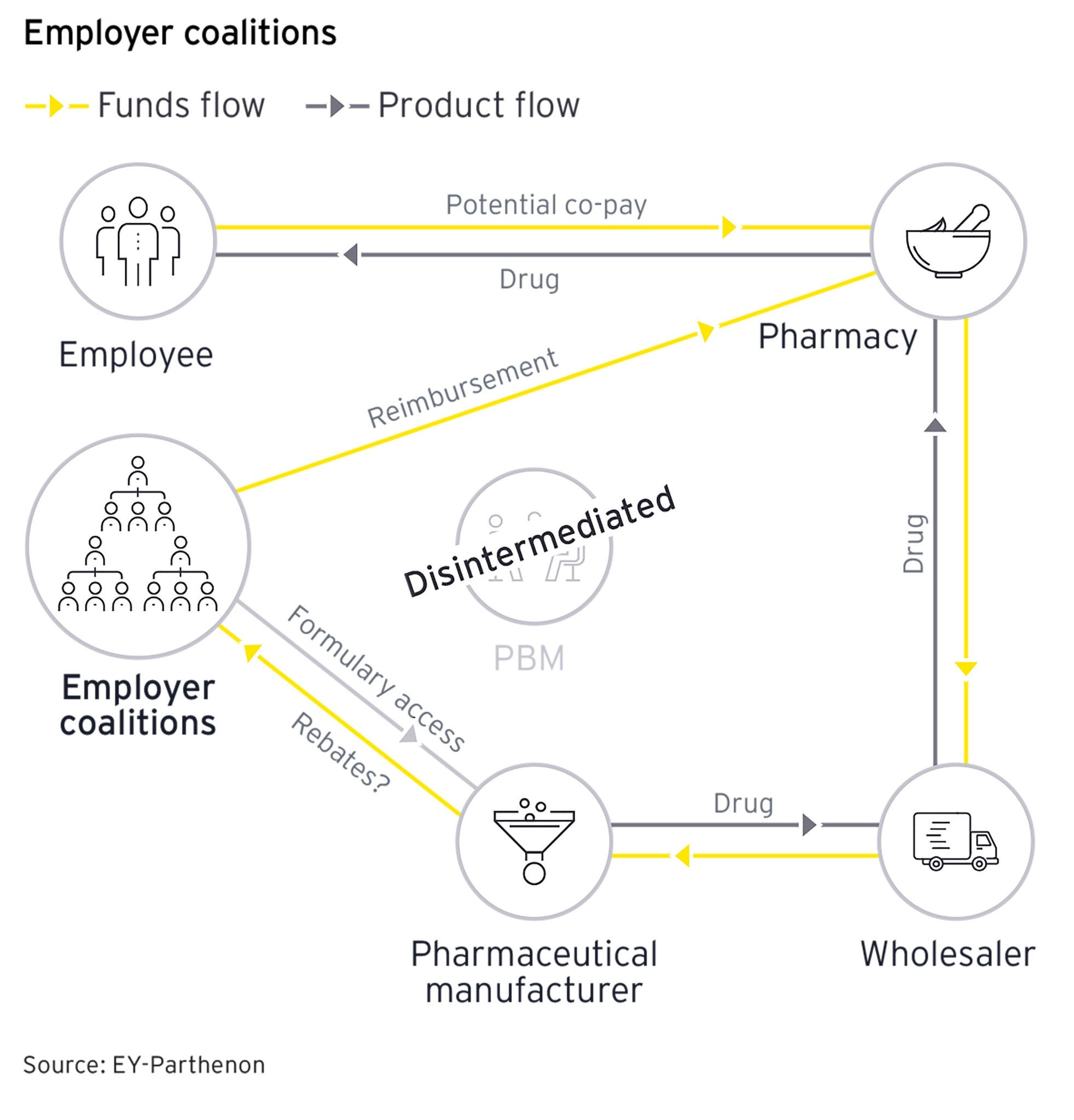
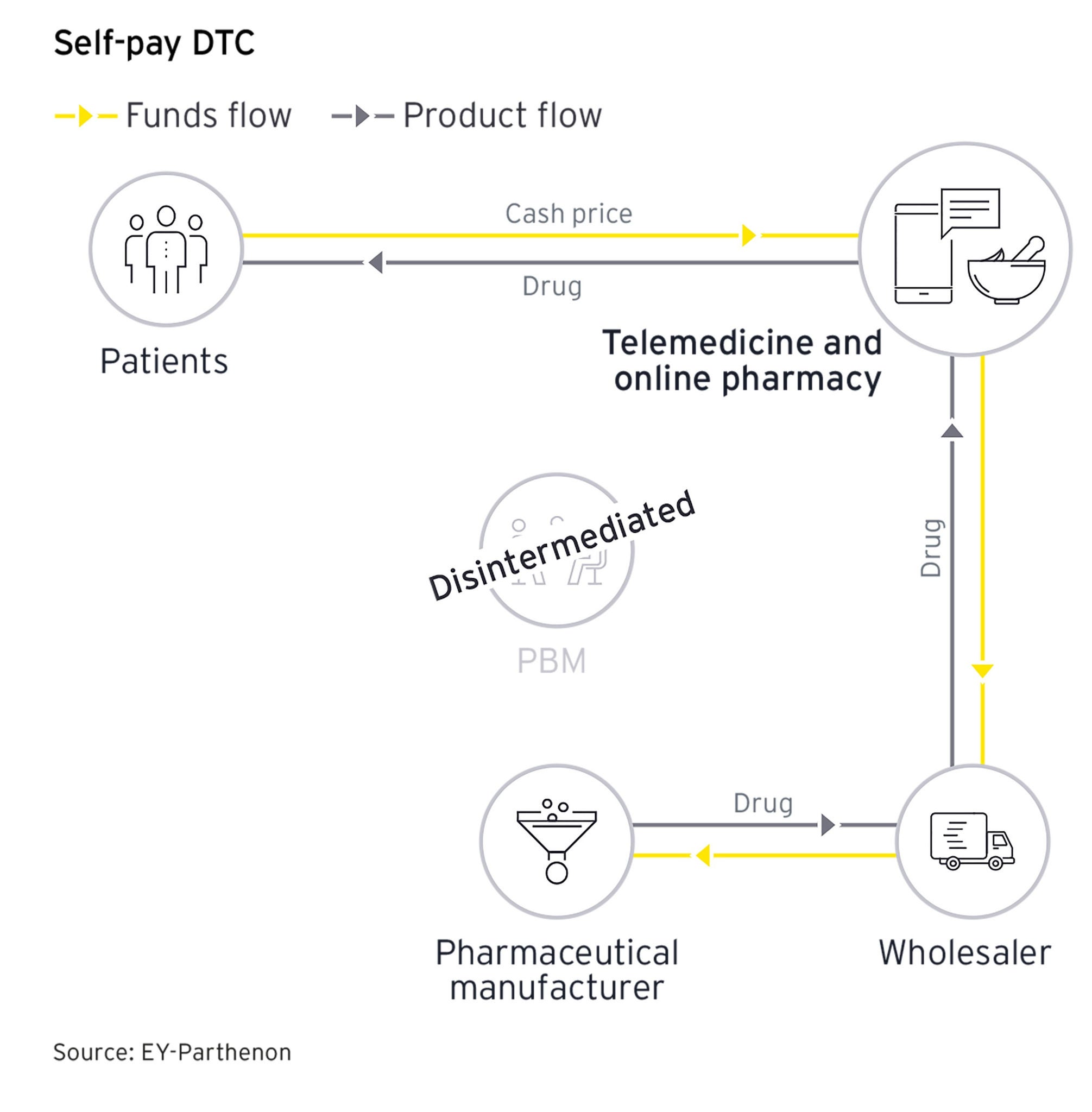
Many employers and pharmaceutical manufacturers are exploring disintermediation strategies that would exclude or limit the role of the PBM in the pharmaceutical value chain. By disintermediating the PBM:
- Employers/plan sponsors hypothesize they can reduce overall spend on high-cost therapies
- Manufacturers expect improved net prices through elimination of rebates and other fees paid to PBMs
These strategies are taking several forms and are likely to serve as a basis for a new paradigm for how high-cost therapies are valued and reimbursed in the future.
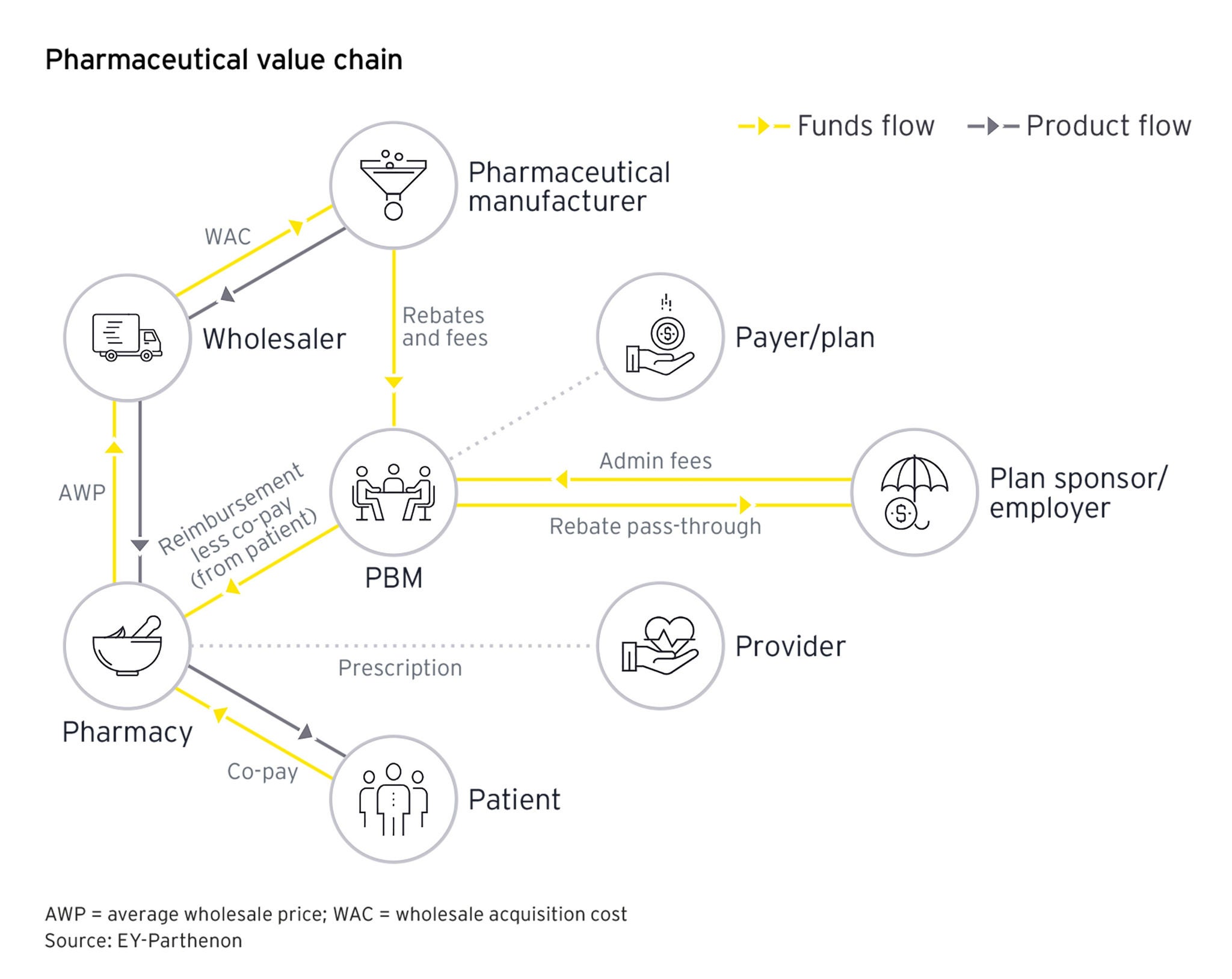
A complex network
PBMs sit at the nexus of many stakeholders across the pharmaceutical value chain due to their financial arrangements with nearly all stakeholders. Employers and plan sponsors, which are the primary customers of PBMs, pay PBMs to manage prescription drug benefit claims processing, formulary design, network access, prior authorizations and other prescription drug benefit design elements. This provides value to employers that do not have prescription drug benefits management as a core competency.
PBMs receive payments, in the form of discounts, rebates and other fees, from manufacturers to secure market access on a formulary (the list of approved drug that a plan sponsor will cover). A conflict of interest arises if PBMs are being paid both by manufacturers and by employers/plan sponsors. These payments may create a dynamic in which the PBM could prioritize access to drugs that have greater rebates and fees from manufacturers at the expense of employers and plan sponsors. While PBMs indicate that most, if not all, rebates are passed through to employers and plan sponsors, employers are skeptical of that assertion. This skepticism has given rise to transparent PBMs that provide greater details of their dealings with manufacturers and several employer coalitions that are attempting to disrupt the model.
Going a step beyond demanding transparency, some employers/plan sponsors and other stakeholders have begun to explore models that fully or partially disintermediate a PBM. The following describes the various models that are being tested in the market.