What lies ahead?
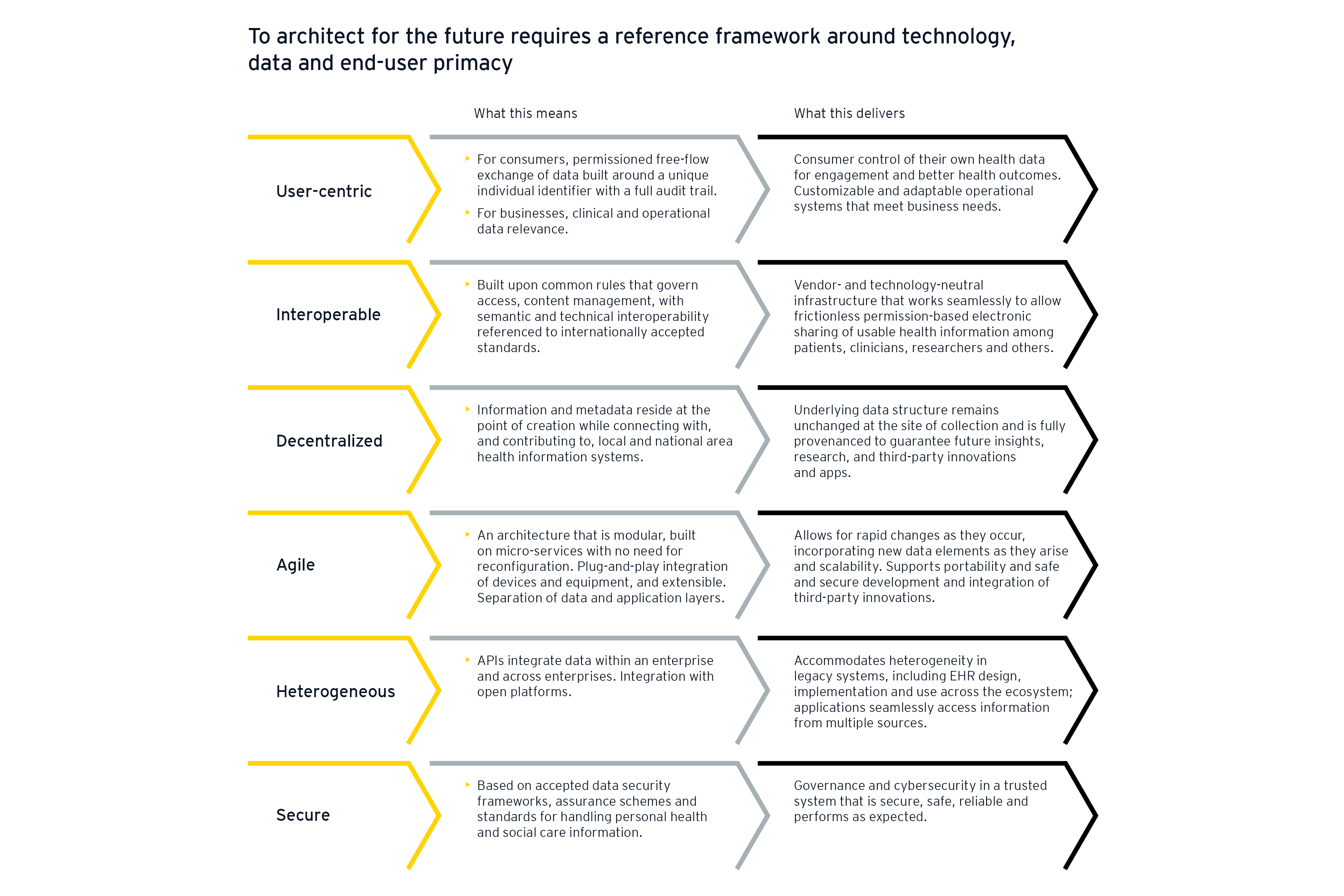
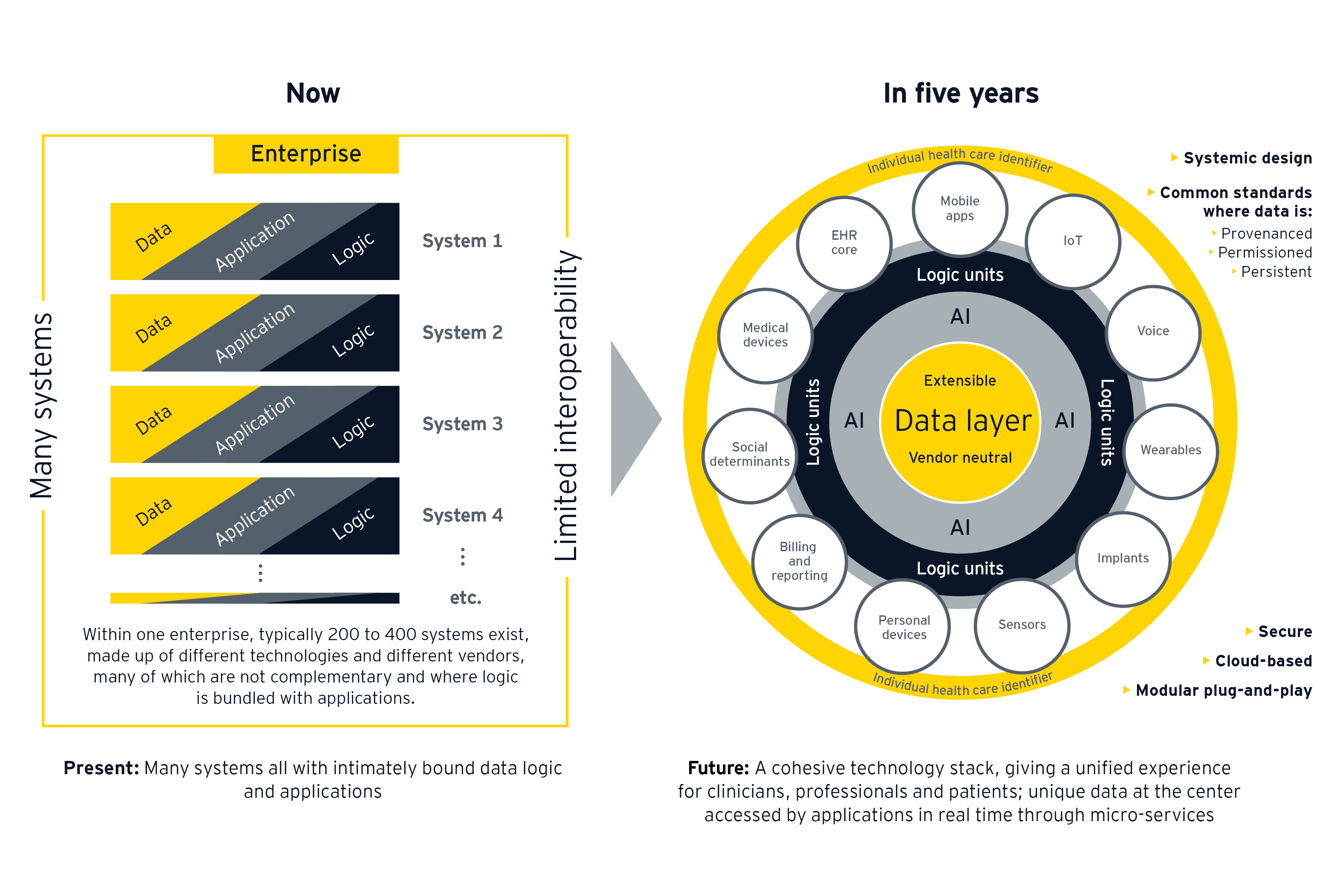
While the overall goal is ecosystem-wide interoperability, there are several steps that health care organizations and policy makers could take today to meet the demands of tomorrow.
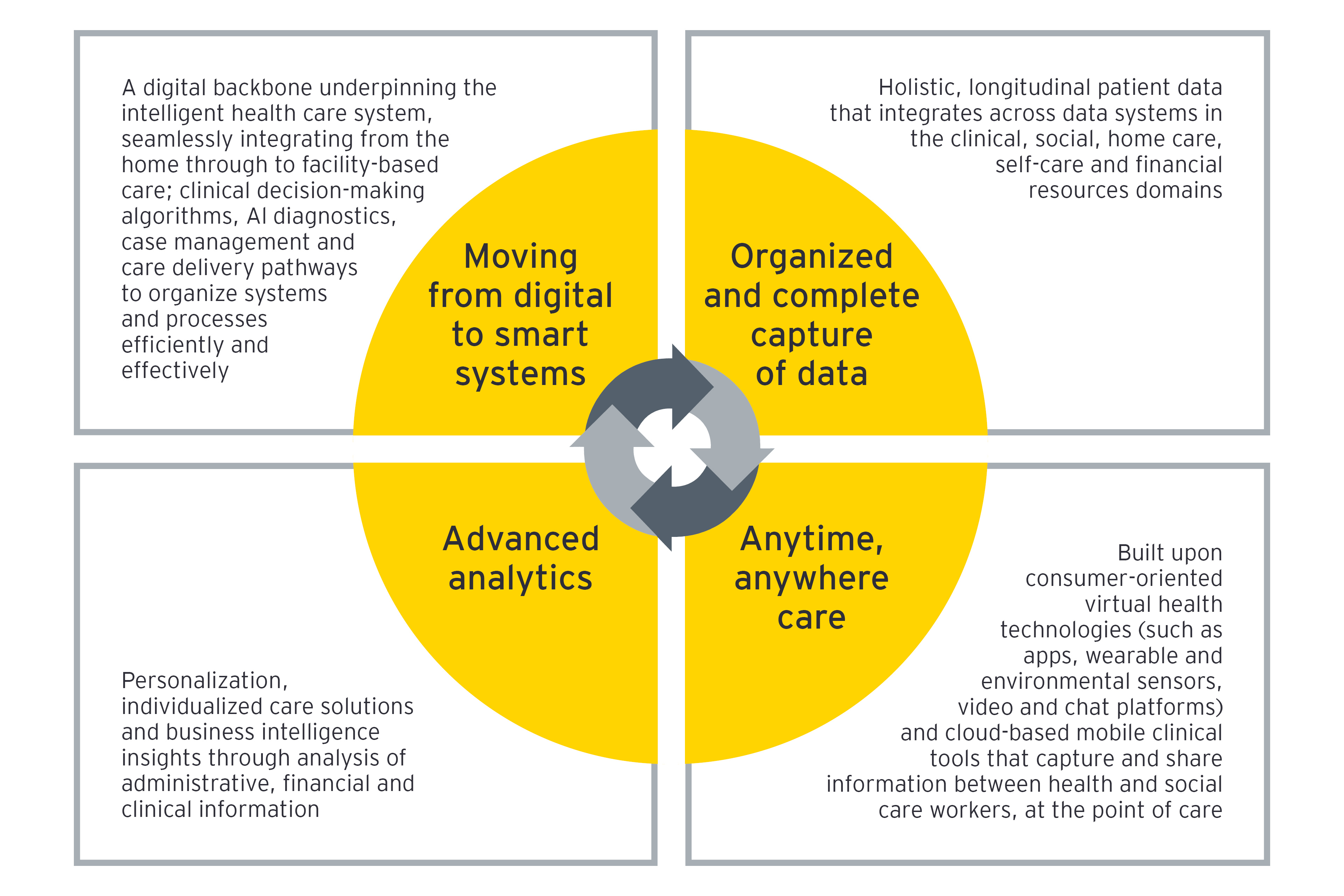
Where we see success in the marketplace is when organizations understand that the way forward is built around data and technologies that grow the business of tomorrow, rather than just a repeat of today’s procurement cycle. These organizations build from an ecosystem mindset, identifying what data is critical and the right strategy to access it. They follow a transformation agenda to create new business models as data becomes the central asset in the organization.
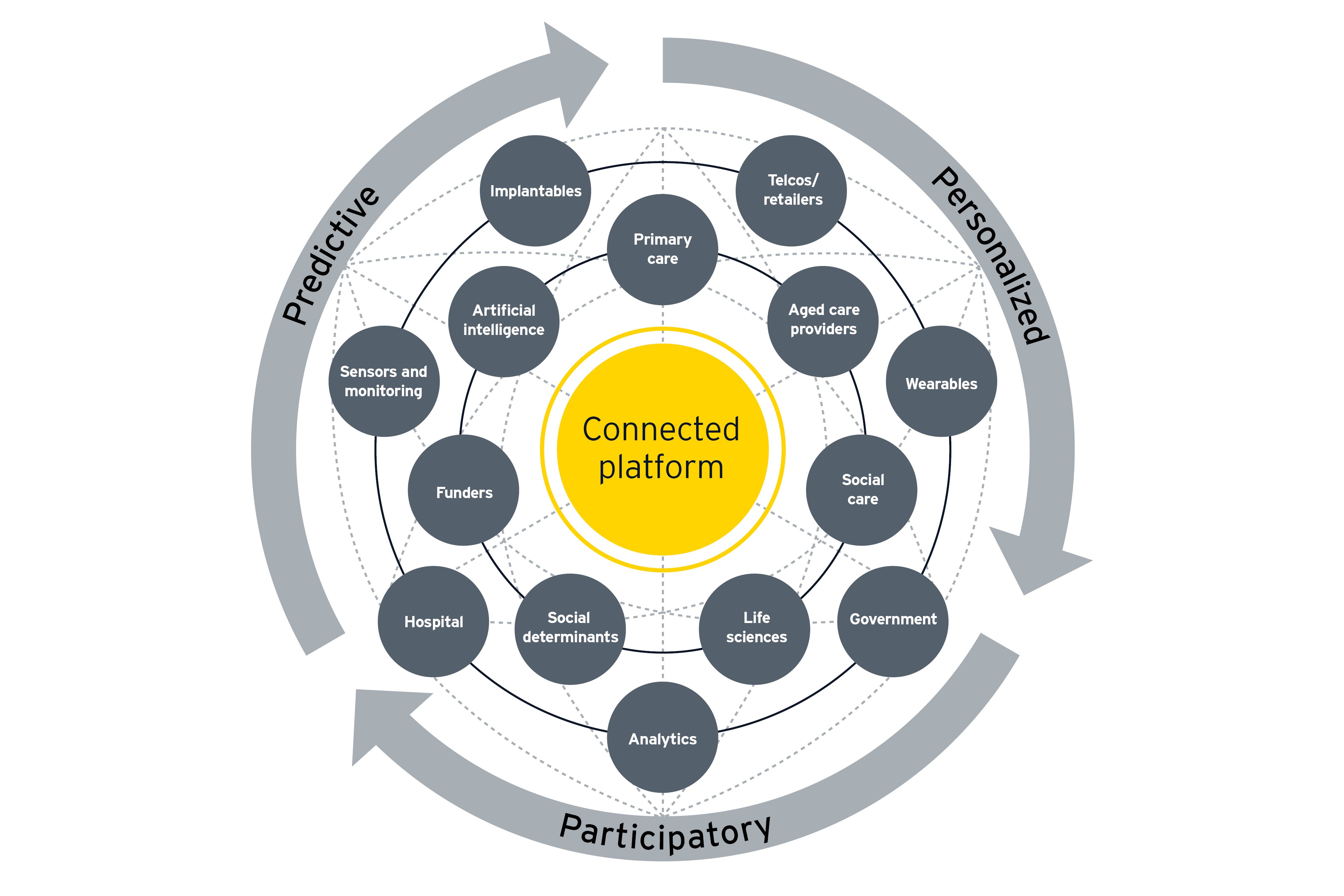
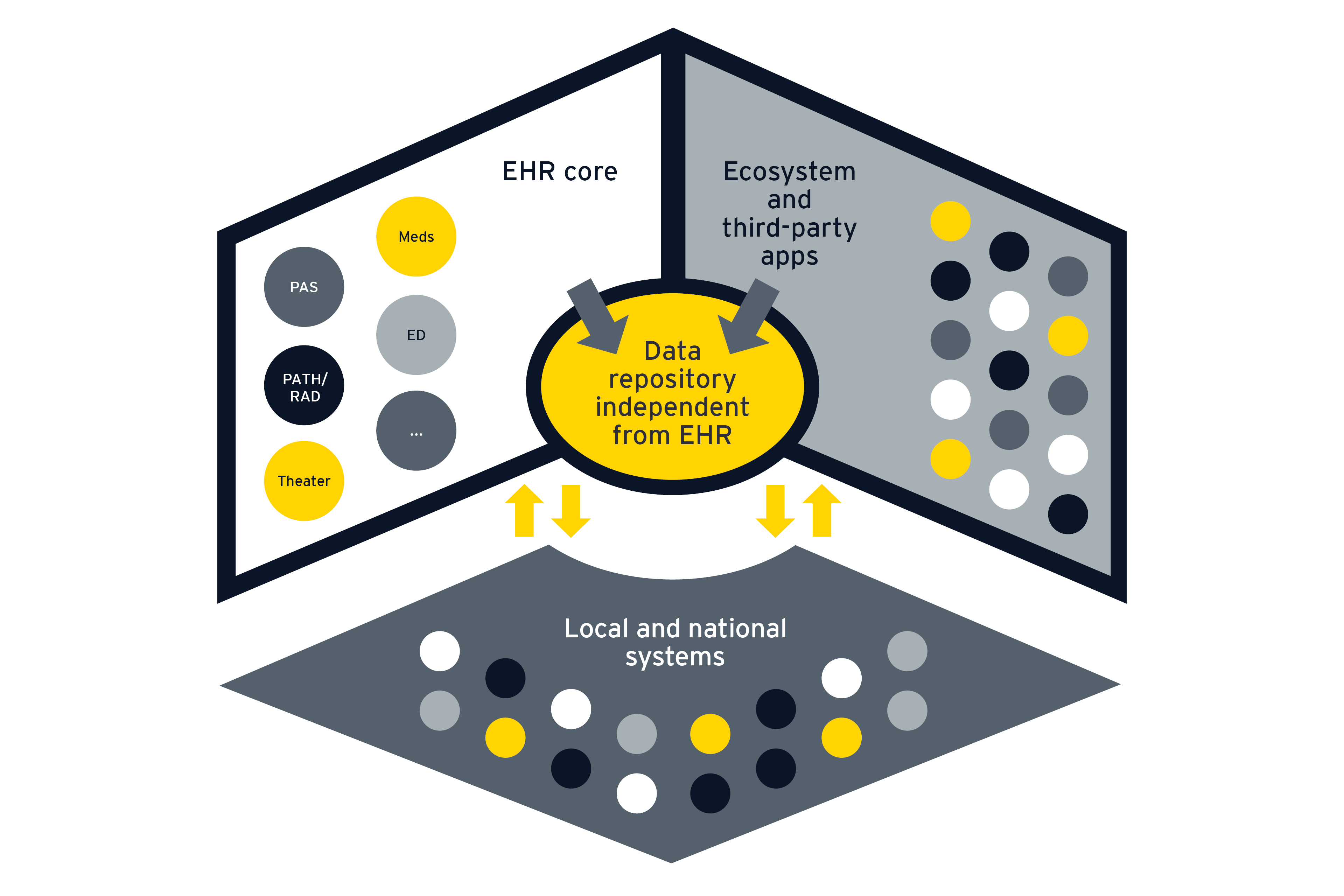
Digital technologies form a data-driven foundation for the future health industry, and conversations about how we can use technology to make a real difference are long overdue. A systemically architected approach for the management of health data is an important step toward a connected health ecosystem, and the technical elements for such a system already exist. To move forward, we will need to reconfigure the information backbone of health care as a new frictionless information architecture, strategically and thoughtfully.
To lay the groundwork for the coming years, here are three things to consider:
1. Framing up the future
The speed of technological change and complexity in the health market require reflecting on purpose, capabilities and priorities.
To find out what creates value and how to get there, ask:
- What lens is your organization looking through? How is purpose defined, and where do value streams lie: with the consumer, the organization or both?
- How will data shape future business models and reimbursement, and what infrastructure must be in place to unlock interaction data and to modernize the employee and consumer experience?
- What risk is involved, and how deep is the appetite for change – incremental steps or redesign from the ground up?
2. How ready is the organization to change?
Future relevance requires agility and confidence to shift, and to do so at scale. But where best to begin? The speed of change is often slow, hampered by contractual obligations, capital-intensive infrastructures and legacy technologies.
To identify the problem, ask:
- What are the pain points to be resolved?
For example, a desire to :
- Drive better clinical outcomes
- Respond to growing demand
- Migrate to new care models and teaming
- Reverse clinician burnout
- Secure revenue streams
- Free investment resources through back-office automation
- Step away from lock-in with longstanding entangled systems
- To what extent does the current tech environment cause or exacerbate the pain points, and how would changing the technology environment resolve the problems?
- What are the opportunities to personalize, simplify and streamline?
3. What is the road map, given the current stage along the technology journey?
Where legacy IT infrastructure exists, the way forward may well lie with maintaining core functionality while investing in adaptable infrastructure such as open architecture and blockchain-enabled solutions that support a connected ecosystem.
To develop the road map, ask:
- What is the plan?
- To optimize existing assets (either by modification or extension); to introduce resources that complement the existing core; or to create a new ecosystem from the ground up
- What is the process?
- A phased transition to new solutions; a greenfield approach of creating new capabilities on a new platform; or a big bang approach that converts all capabilities to a modernized solution in single or multiple events
- What else must be done?
- Design for trust, governance and align organizational culture - where boards, clinical and organizational leadership are comfortable with creating friction and deviating from the status quo, and have the skills to do so
- Bring other stakeholders, including the board and policy makers, along on the journey
- Build the right in-house team with right capabilities to execute