EY se refiere a la organización global, y puede referirse a una o más, de las firmas miembro de Ernst & Young Global Limited, cada una de las cuales es una entidad legal independiente. Ernst & Young Global Limited, una compañía británica limitada por garantía, no brinda servicios a los clientes.

Las buenas experiencias del consumidor fluyen hacia mejores experiencias de fuerza laboral y viceversa. Ambos son buenos para los negocios.
Tres preguntas para hacer
- ¿Cómo se diferenciará nuestra organización con respecto a las experiencias de los pacientes y la fuerza laboral para competir en el futuro?
- ¿Cómo identificará nuestra organización a los socios potenciales para diferenciar nuestras ofertas de modo que creemos las experiencias del cliente del futuro y que nuestros productos y servicios se destaquen?
- ¿Qué cambios necesitamos hacer en nuestras capacidades, sistemas, infraestructura y tecnología, cultura organizacional y comportamientos para obtener los resultados que buscamos?
Las buenas experiencias del consumidor fluyen hacia mejores experiencias de fuerza laboral y viceversa. Ambos son buenos para los negocios y deben ser una prioridad para todas las organizaciones de atención médica. La conclusión es que las organizaciones de atención médica necesitan una perspectiva de toda la empresa que incluya a las personas en ambos lados de la ecuación de la prestación de atención para permitir la mejor y más eficiente atención, en el lugar correcto y en el momento correcto.
Para los consumidores de atención médica, las experiencias positivas pueden afectar los resultados de la atención, la relación continua con el proveedor de atención médica y la probabilidad de adherirse al tratamiento, así como de buscar atención de manera proactiva en el futuro. El diseño de vías de atención más inteligentes facilita que los consumidores se involucren con la salud para la prevención, en lugar de solo cuando están enfermos. Esto se extiende a las infraestructuras que apoyan el cambio de comportamiento durante períodos prolongados y también facilitan la recopilación de datos de bajo esfuerzo, incluida la integración de los datos de determinantes sociales con los clínicos, para obtener mejores resultados.
Para la fuerza laboral, la experiencia de salud inteligente comienza con la transformación digital de la empresa, de la que hablamos en otros artículos de esta serie de Smart Health. En combinación, la tecnología de salud inteligente, junto con el toque humano, ofrece la oportunidad de cambiar la prestación de atención de maneras que son importantes tanto para los médicos como para los pacientes.
Los conjuntos de datos longitudinales completos, el flujo de datos mejorado y la coordinación de la atención inherente a los sistemas de salud inteligentes generan información para pacientes y médicos. Esto incluye cosas como vías de atención individualizadas para el manejo de enfermedades crónicas y la participación conductual a través de herramientas habilitadas para inteligencia artificial (IA).
La digitalización y automatización de los procesos existentes puede reducir las tareas repetitivas y de bajo valor, liberando tiempo y energía del personal para la participación del paciente y la atención clínica1.Estas tecnologías impulsan soluciones innovadoras que pueden reducir la carga del personal y reducir el agotamiento y la rotación2.La productividad clínica puede mejorarse a medida que la rápida difusión de las mejores prácticas y la medicina basada en la evidencia pueden cambiar hábitos profundamente arraigados y reducir la variabilidad y el desperdicio, y mejorar los resultados de los pacientes3.
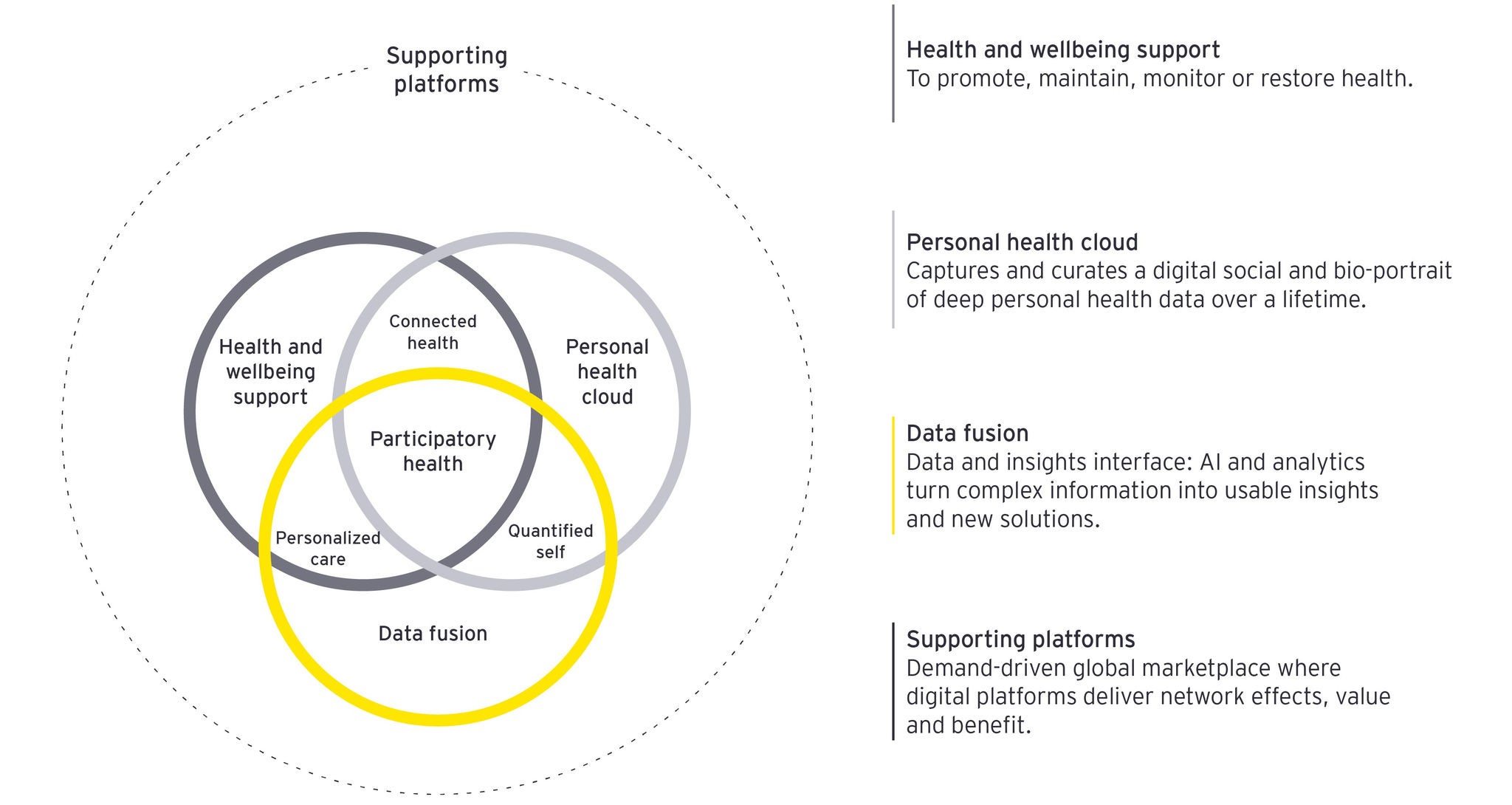
A medida que avanzamos hacia la próxima generación de atención médica, el modelo de atención está cambiando a uno preventivo, personalizado y participativo (Figura 1). El sistema de salud del futuro estará conectado digitalmente, centrado en el consumidor y centrado en el bienestar. Las herramientas de participación del paciente, la atención virtual, los hogares inteligentes y la analítica impulsada por IA brindarán a las personas las herramientas para administrar su salud, elecciones de estilo de vida y afecciones crónicas de maneras muy diferentes.
Las tecnologías que mejoran la experiencia de un extremo a otro y eliminan los silos conectando el continuo de la atención son solo una parte de la solución. El otro es un enfoque implacable en el lado humano de la atención. Obtener la experiencia correcta significa comprender y valorar a las personas por lo que son y el conjunto único de necesidades, específicas para el viaje de salud y bienestar de cada individuo.
Para los consumidores, esto significa tratar a las personas como individuos a través de una atención altamente personalizada y un compromiso proactivo que se adapte a ellos, o a la "N de 1" y, para la fuerza laboral, un compromiso significativo con su trabajo en un entorno de baja fricción, altamente modernizado e inspirador.
Figura 1: Un paradigma participativo de la salud
Descarga el artículo en pdf
Tres principios para diseñar una experiencia de salud inteligente
Establecer las bases para una organización más receptiva y eficiente, incluidas las experiencias y condiciones de trabajo modernizadas que los pacientes y el personal de salud desean, significa considerar lo siguiente:
1. Una visión basada en experiencias altamente personalizadas
La personalización es fundamental para una experiencia de cliente excepcional. Da forma a cada punto de conexión a lo largo de una ruta de atención que atiende las necesidades y preferencias distintivas del consumidor individual, o cuida a un N de 1. La atención se adapta para abordar el historial médico único de cada individuo. Por ejemplo, el conocimiento del historial de salud de una persona, junto con un registro longitudinal de datos de salud, permite una atención altamente personalizada. Una lectura de hipertensión puede estar dentro de un rango considerado aceptable en el contexto de la historia de una persona, pero generar una alerta para otra persona.
La participación de los consumidores con el sistema de salud varía mucho y, a medida que el sistema de salud se vuelve altamente digitalizado e hiperconectado, las actitudes y creencias subyacentes sobre las tecnologías de salud pueden influir fundamentalmente en las interacciones y, en última instancia, en los resultados. En una investigación reciente, EY identificó cuatro segmentos únicos de consumidores de atención médica en Estados Unidos que atraviesan grupos demográficos que tienen actitudes y comportamientos distintivos con respecto a las tecnologías de salud del consumidor.
Dos segmentos reflejan una perspectiva desinteresada, incluidos los pesimistas y los escépticos, los cuales tienen diferentes niveles de desinterés e incomodidad con el uso de las tecnologías de salud del consumidor. En el otro lado se encuentran los arquetipos conectados, donde los segmentos de mente abierta y optimista son receptivos y, en mayor medida, han adoptado la integración de las tecnologías de salud digital en su vida cotidiana (Figura 2).
Figura 2: Cuatro segmentos de consumidores de atención médica en Estados Unidos: Entusiasmo por la tecnología de salud del consumidor
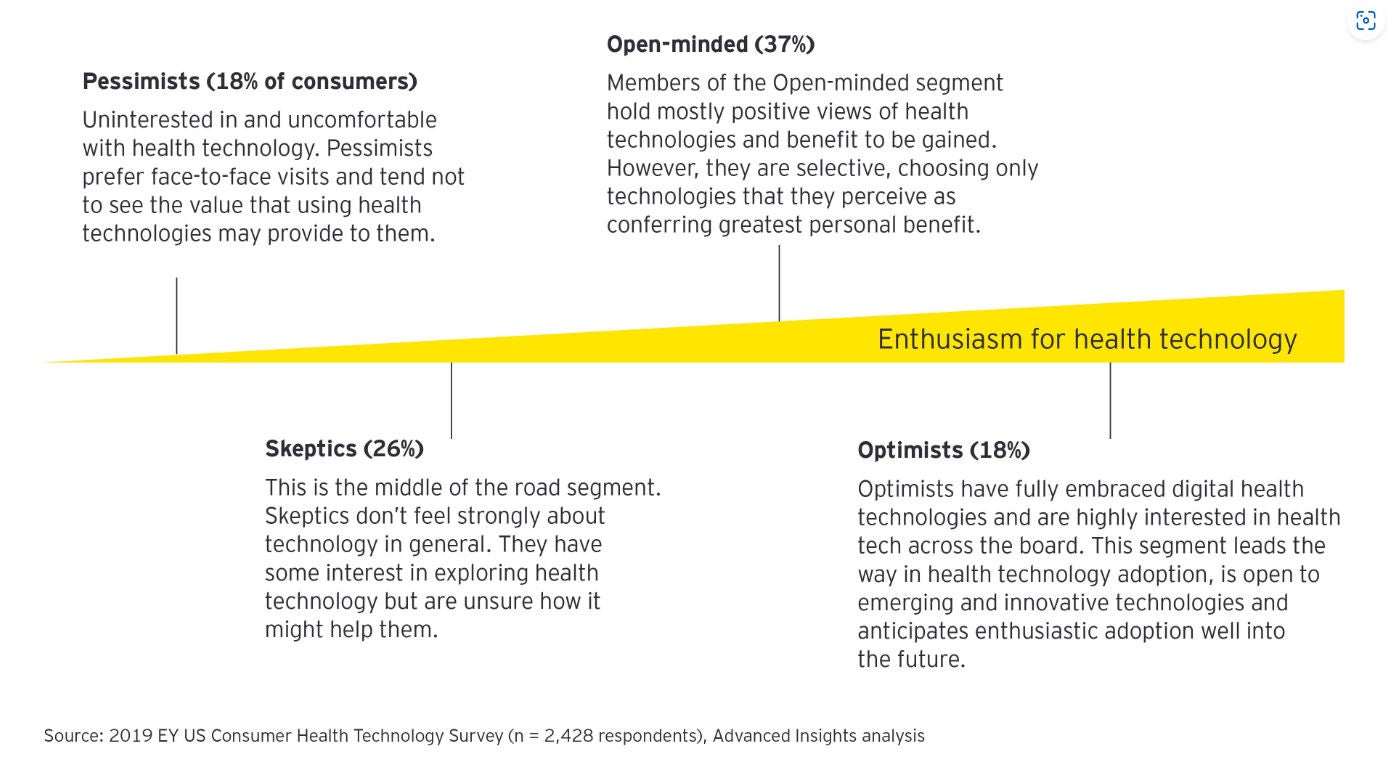
Comprender la combinación de segmentos, como estos, en las poblaciones puede dar lugar a información valiosa sobre cómo orientar y personalizar los productos, servicios e información para las poblaciones de pacientes. Se pueden diseñar innovaciones de productos y servicios altamente específicas utilizando análisis de datos sofisticados de las preferencias, comportamientos y propensión a participar de los consumidores. Estos pueden estratificarse aún más según el estado de salud, los patrones de utilización de la atención y la información sobre los determinantes sociales.
2. Un buen diseño comienza y termina con las personas
El diseño centrado en el ser humano es simplemente diseñar con y para las personas. Es un enfoque creativo para la resolución de problemas; Las personas están en el centro y comienza con una investigación exploratoria e inmersiva. Hacer preguntas inteligentes y de sondeo que desafíen las creencias mantenidas en torno al statu quo y pasar tiempo con personas en el entorno del mundo real son los puntos de partida de un viaje de descubrimiento. Este es uno que se mueve a lo largo de varias etapas clave de exploración de lo que se debe hacer, imaginando nuevas formas de abordar el desafío definido y probando las suposiciones a través de la creación de prototipos con usuarios potenciales y el rediseño iterativo (ver Figura 3).
Las organizaciones de atención médica pueden ser especialmente grandes y complejas, y las soluciones deben funcionar para las personas, y no al revés. Los mejores resultados surgen a través de un proceso de codiseño participativo, donde los consumidores y trabajadores de la atención médica imaginan cómo podría ser una mejor experiencia para todos4.
Por ejemplo, esto puede ser muy enfocado, como la racionalización de una vía de atención o un protocolo de alta para una mayor eficiencia y comodidad. O puede impugnar supuestos de larga data y formas habituales de pensar para cambiar radicalmente los procesos y el diseño de servicios para redefinir el valor, cambiar a nuevos mercados o modelos de negocio, introducir un cambio cultural organizacional complejo o abordar los desafíos iniciales relacionados con los determinantes sociales de la salud.
Un ejemplo de ello podría ser la reinvención de la forma en que las soluciones de atención sanitaria pueden trasladarse del hospital al hogar o a la comunidad y reducir las desigualdades en materia de salud mejorando el acceso a la atención.
Un ejemplo interesante del potencial del diseño centrado en el ser humano es el de los caminos del deseo, o los atajos espontáneos que toman las personas, generalmente la ruta más corta o la más fácil de navegar. El uso de este tipo de información para informar la planificación del sitio se ha llevado a cabo en varias instituciones educativas de los Estados Unidos. mediante la observación de las rutas naturales de caminata creadas por los estudiantes, antes de colocar las aceras5.
Encontrar los caminos preferidos o deseados en la atención médica puede ayudar a diseñar servicios más receptivos y eficientes que satisfagan mejor las necesidades de los pacientes, los cuidadores y la fuerza laboral. La ubicación conjunta de servicios relacionados con el tema, por ejemplo, servicios torácicos o servicios de emergencia, puede permitir una mayor eficiencia en el flujo de trabajo, distancias de viaje más cortas para el personal y los pacientes, y acceso justo a tiempo a los equipos6.
Esto también puede aplicarse al diseño de programas, como los servicios de salud mental rurales y remotos, prestados de manera que las personas realmente los utilicen, en lugar de la implementación de arriba hacia abajo de estructuras predeterminadas7.
Figura 3: Diseño centrado en el ser humano para el cuidado de la salud

3. Activos digitales y análisis
Los activos digitales son facilitadores clave de la atención holística. Diseñar para una experiencia más humanista con interfaces digitales significa comprender completamente las formas en que las personas interactúan con los dispositivos y las tecnologías. Un ejemplo es el diseño de nuevas tecnologías altamente innovadoras, como las tecnologías hápticas multisensoriales. Estos humanizan aún más la experiencia digital a través de la retroalimentación táctil a los usuarios, incluidos los dispositivos portátiles de consumo y la educación clínica, como la capacitación quirúrgica.
Las herramientas y tecnologías digitales impulsan la estandarización de los procesos para la prestación de servicios y reducen el desperdicio y la atención innecesaria a través de vías de atención clínica integradas. Esto también conducirá a suavizar algunos de los puntos débiles en la experiencia del paciente y la carga impuesta por el sistema a los pacientes.
Estas incluyen:
- Automatización inteligente de tareas manuales repetitivas y uso de robótica para estandarizar y sistematizar procesos para optimizar la eficiencia operativa e impulsar la productividad de la fuerza laboral
- Información sobre el comportamiento del consumidor que surge a través de la captura y el análisis de una gran cantidad de datos relacionados con la salud, como los resultados de salud, la prescripción, los seguros, los datos generados por el consumidor y la genética para formar la base de la atención médica predictiva, preventiva y personalizada.
- Análisis de datos para mejorar la comprensión del recorrido de la enfermedad y estimular las vastas posibilidades de desarrollo de disciplinas, incluidas la biología y la medicina de sistemas integrativos, la informática biomédica, la investigación traslacional y la salud de la población.
- Síntesis de los sistemas de back y front office para permitir una programación, comunicaciones, facturación y pago más convenientes
- Una réplica digital de los activos físicos y los procesos organizativos para la supervisión en tiempo real, la resolución de problemas y las pruebas de simulación.
En el sistema de salud inteligente del futuro, un enfoque en mejorar la experiencia del paciente y de la fuerza laboral será clave.
Colaboradores: Rachel Hall, Líder Global de Experiencia en Salud Inteligente de EY; Kenny O'Neill, estratega de experiencia de salud inteligente de EY; Aakanksha Kaul, analista de ciencias de la salud y bienestar global de EY
Resumen
Prestar atención al cliente tiene un sólido sentido clínico y comercial. Lo que debemos comprender en profundidad son los beneficios que se obtendrán al mejorar la experiencia de un extremo a otro en un viaje de atención médica integral tanto para los consumidores como para el personal sanitario. En el sistema de salud inteligente del futuro, un enfoque en mejorar la experiencia del paciente y de la fuerza laboral será clave. Las tecnologías que mejoran la experiencia de un extremo a otro y eliminan los silos conectando el continuo de la atención son solo una parte de la solución. El otro es prestar atención sistemáticamente al lado humano del cuidado para que la experiencia sea la correcta.
Artículos relacionados
Interconnecting people, the environment, and systems is where health becomes smart. Highly interdependent, one can’t live without the other.
What connections will move health from reimagining to reality?
In the 2019 edition of New Horizons, we explore how the health sector can begin executing on a new vision of a connected health ecosystem.