Chapter 1
Awareness and prevention
Awareness landscape in India is dominated by tobacco and tobacco-related cancers. Knowledge of other common cancers such as cervical is low.
Few people in India seemed to be concerned about cancer compared to other countries, implying a general attitude of indifference towards cancer. As per the UICC global survey, only 43% respondents in India indicated that they were concerned or somewhat concerned about developing cancer in their lifetime compared to a global average of 58%.
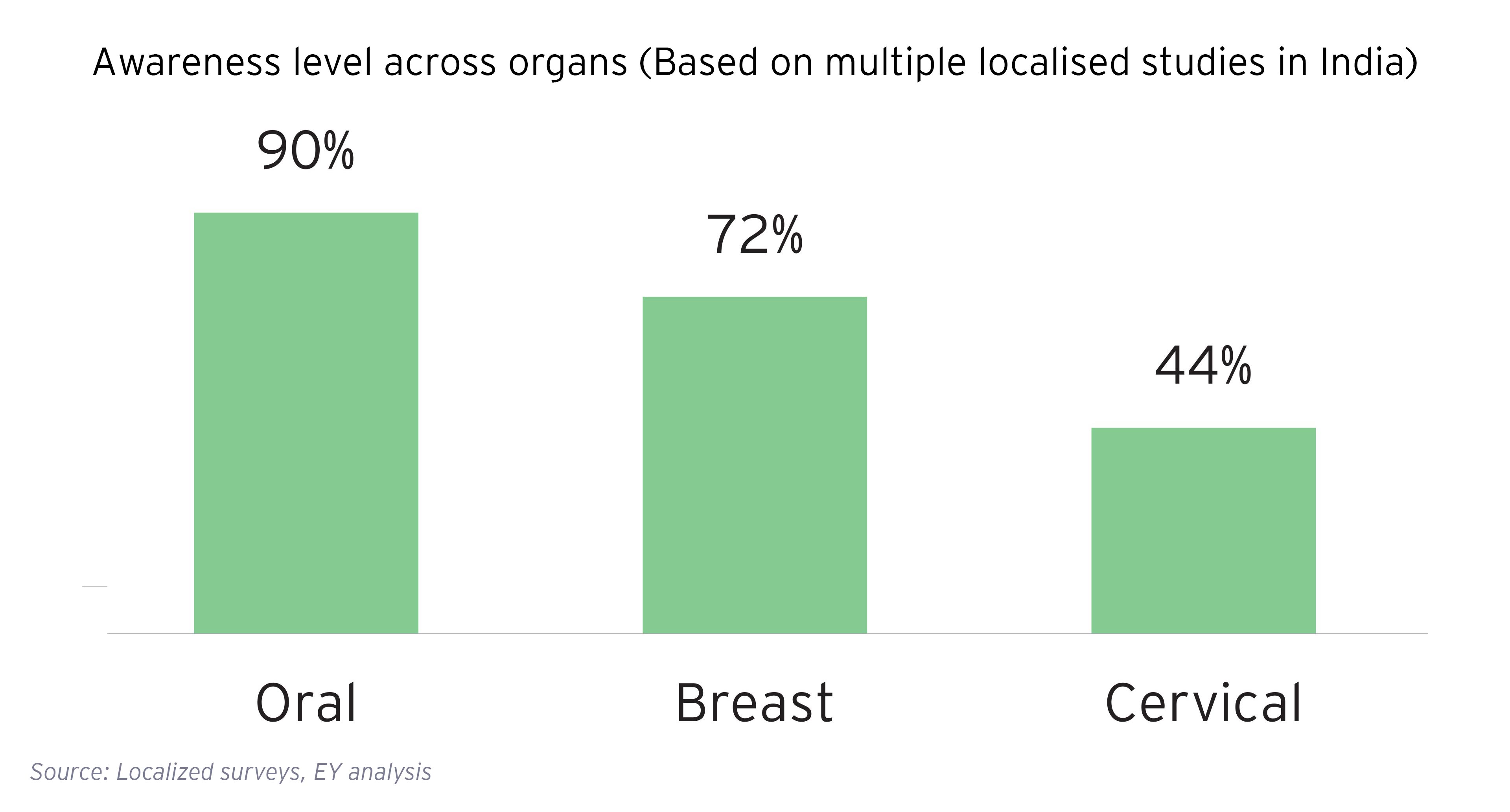
Uptake of screening for breast, cervical and oral cancer and HPV vaccination is very low despite moderate levels of awareness.
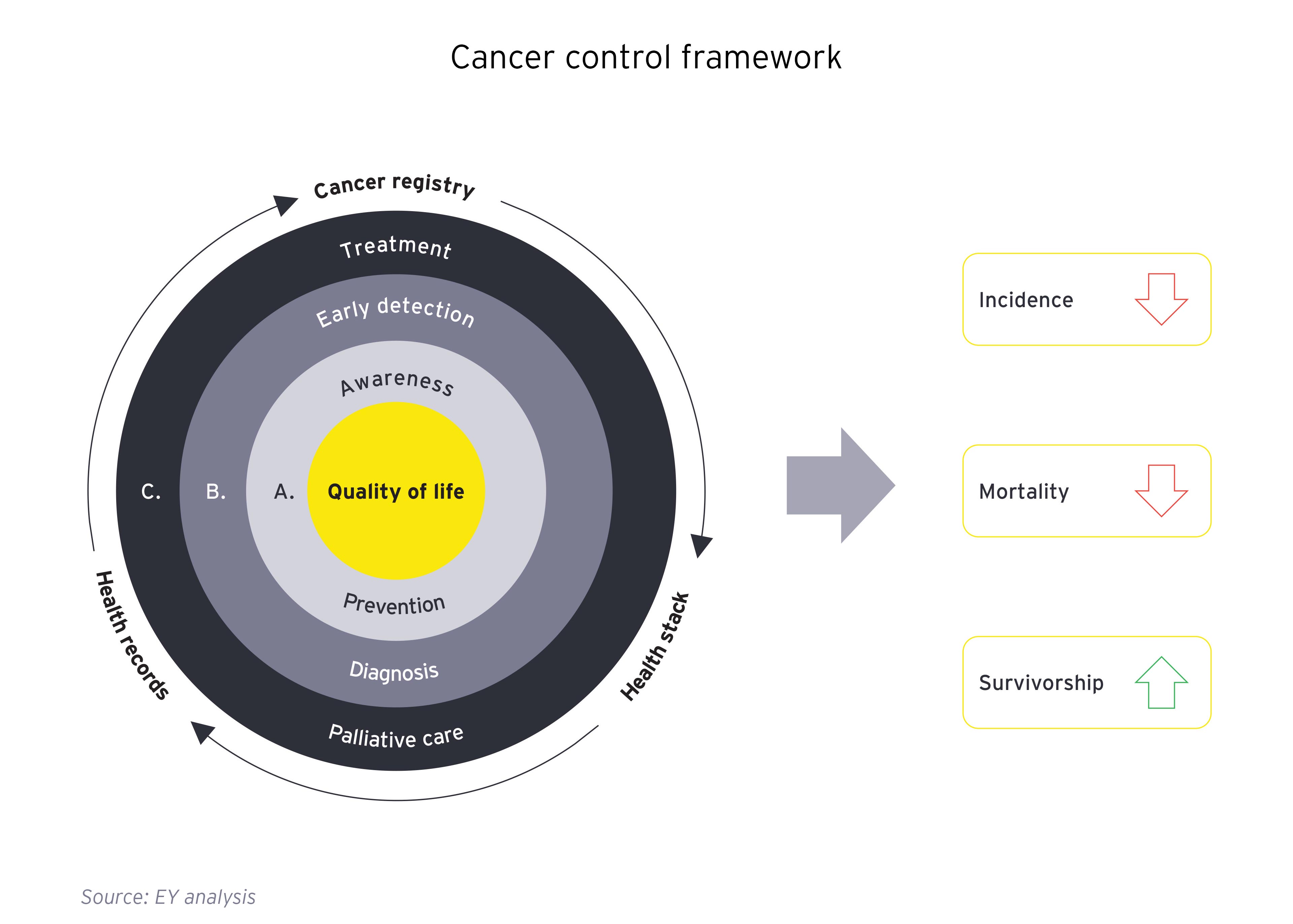
Primary prevention involves limiting exposure to carcinogenic risk factors. While there are several carcinogenic risk factors, modifiable risk factors such as tobacco, alcohol, obesity, infectious and environmental factors are amenable to prevention. While India undertook several policy measures to reduce exposure to risk factors, there is still significant progress required.

Chapter 2
Detection and diagnosis
It is crucial that cancer prevention and early diagnosis are prioritized by society, governments, and the healthcare ecosystem.
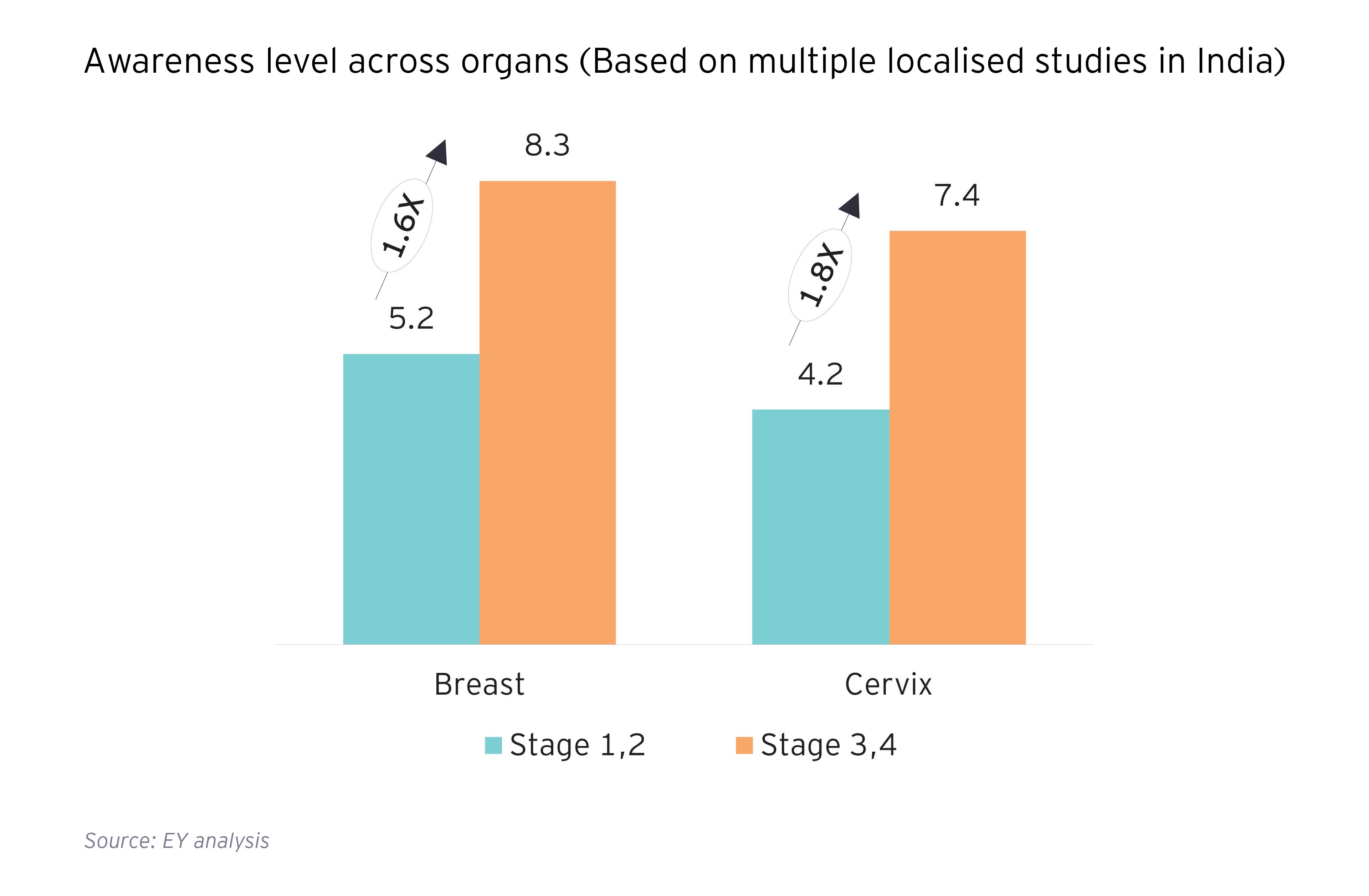
Despite the proven benefits of early identification for downstaging the disease as well as in achieving a reduction in mortality and morbidity, screening penetration of key cancers in India is very low: Across focus cancers being screened under the National Programme for Prevention and Control of Cancer, Diabetes, Cardiovascular diseases and Stroke (NPCDCS), screening coverage is less than 5% of population which is negligible when compared with global peers. Capacity constraints in terms of physical infrastructure and workforce, lack of training of the methods for cancer screening among healthcare workers and deficiencies in referral mechanism are key roadblocks to the success of the programme. Additionally, lack of data capture to maintain longitudinal health records of population right from screening stage and ensuring tracking and follow up with patients for effective referrals is a key deterrent in the expansion and penetration of screening programs.
Prevent, screen and spread awareness with least anxiety, low cost and avoiding unnecessary stigma of cancer. Treat with goal of the basic choice, early access and modest cost.

Chapter 3
Treatment including palliative care
There is significant geographic skew in the presence of comprehensive cancer centers in the country.
Only ~175 districts in the country covering 40-45% of the population have Comprehensive Cancer Centres (CCCs)1 . Of the 470 to 480 CCs available in the country ~40% are concentrated in metros and state capitals. Severe gap continues in access to radiotherapy (RT) treatment in the country with RT per million population of 0.4 vis-à-vis WHO recommendation of 1 RT per million population.
Affordability of treatment
Treatment cost for cancer care is financially prohibitive and is almost 3x that of other non-communicable diseases (NCD). Additionally, treatment cost has been increasing with the cost of a single cancer hospitalization (in public or private facility) exceeding average annual expenditure of 80% population in 2017 vis-à-vis 60% population in 2014.
The complex challenges of the cancer control landscape in India are further worsened by the lack of comprehensive data w.r.t to incidence and mortality which is representative of the Indian population. The population and hospital-based cancer registries set up four decades ago, have so far been able to cover only 10% of the population of the country with several states such as Uttar Pradesh, Madhya Pradesh, Andhra Pradesh, Rajasthan, Telangana and Orissa having inadequate presence and penetration of registries2.
The challenges in the current system of cancer disease management in the country have been further corroborated by a survey carried out with 154 cancer patients and care givers. Gaps in the patient journey were characterized into seven key themes which need to be addressed to improve experience and satisfaction of cancer patients in the country:
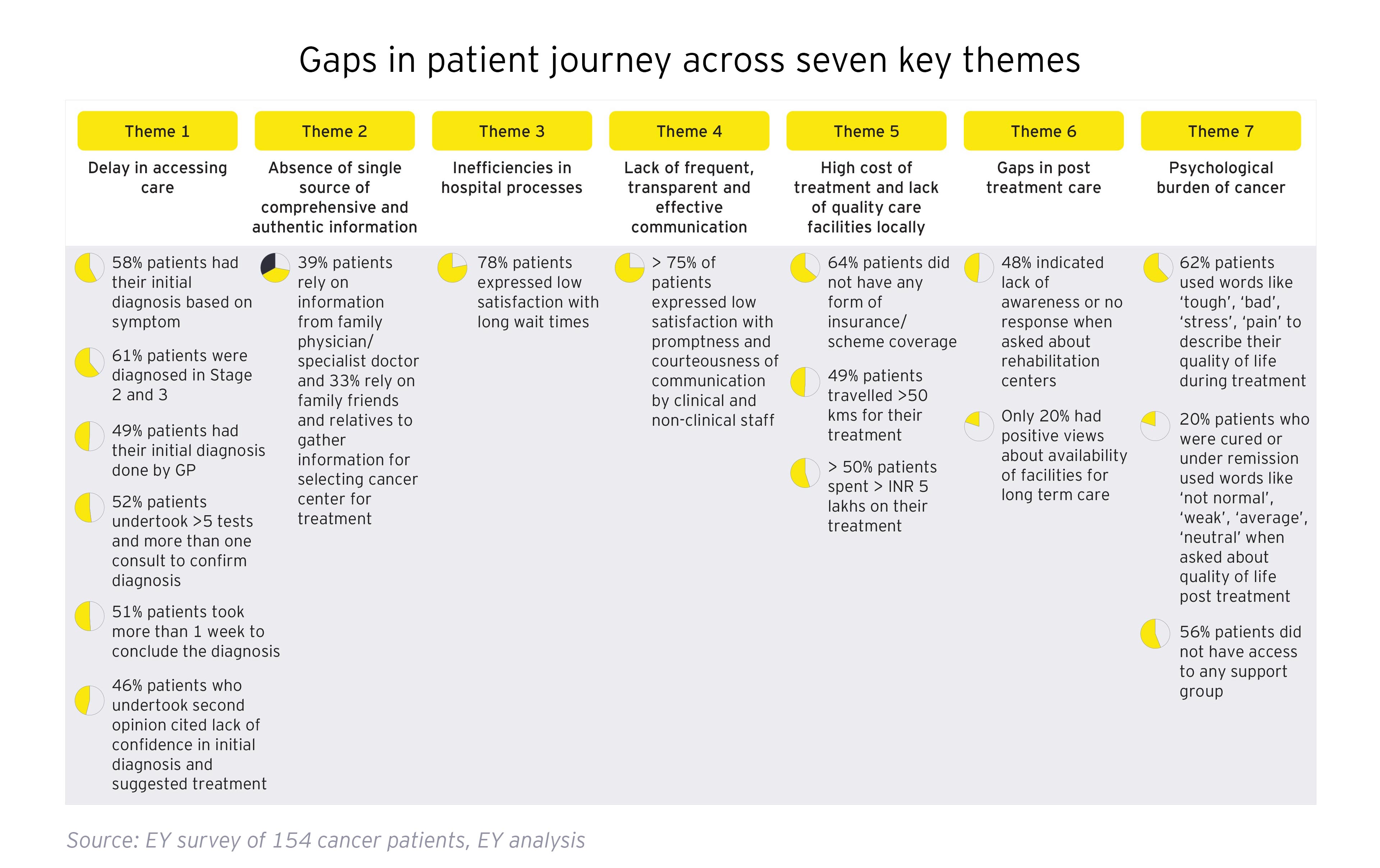
Some of the most cutting-edge cancer treatment methods and technology are available in our country. However, we have a long way to go before we can ensure that cancer patients from every socioeconomic background receive the best possible care. In addition to treatment, we must also take into account leveraging technology to close the care gaps associated with accessibility and affordability. Telemedicine, electronic patient records, robotics, AI-backed upskilling methods, daycare chemo, home care etc., are some of the strategies that are already in place to address these care gaps.
Additionally, capacity and capability building, resource stratification around models of care, and workforce planning have been popular themes for discussion and analysis. India has to further expand its complete cancer care infrastructure, including prevention, care delivery, skilled workforce, technology, and equipment, in order to increase its capacity and capabilities for treating and managing cancer. To make cancer care more effective and affordable for the entire population, we must improve workflow efficiency and treatment outcomes. Using its trademark ingenuity and frugality, India has an opportunity to find innovative solutions to bridge the existing care gaps for her citizens and to guide other developing and developed nations.
Comprehensive and integrated approach by a multidisciplinary team is the key to deliver best outcome for cancer treatment. What works for a patient will work for the nation. Collaboration among all stakeholders is imperative to effectively address India's growing cancer burden.
Related content
Summary
To make cancer care more effective and affordable for the entire population, we must improve workflow efficiency and treatment outcomes. Using its trademark ingenuity and frugality, India has an opportunity to find innovative solutions to bridge the existing care gaps for her citizens and to guide other developing and developed nations.