EY refers to the global organization, and may refer to one or more, of the member firms of Ernst & Young Global Limited, each of which is a separate legal entity. Ernst & Young Global Limited, a UK company limited by guarantee, does not provide services to clients.
How EY can help
-
The EY Health Outcomes Platform aligns all stakeholders by providing a practical solution to operate value-based contracts at scale. Find out how.
Read more
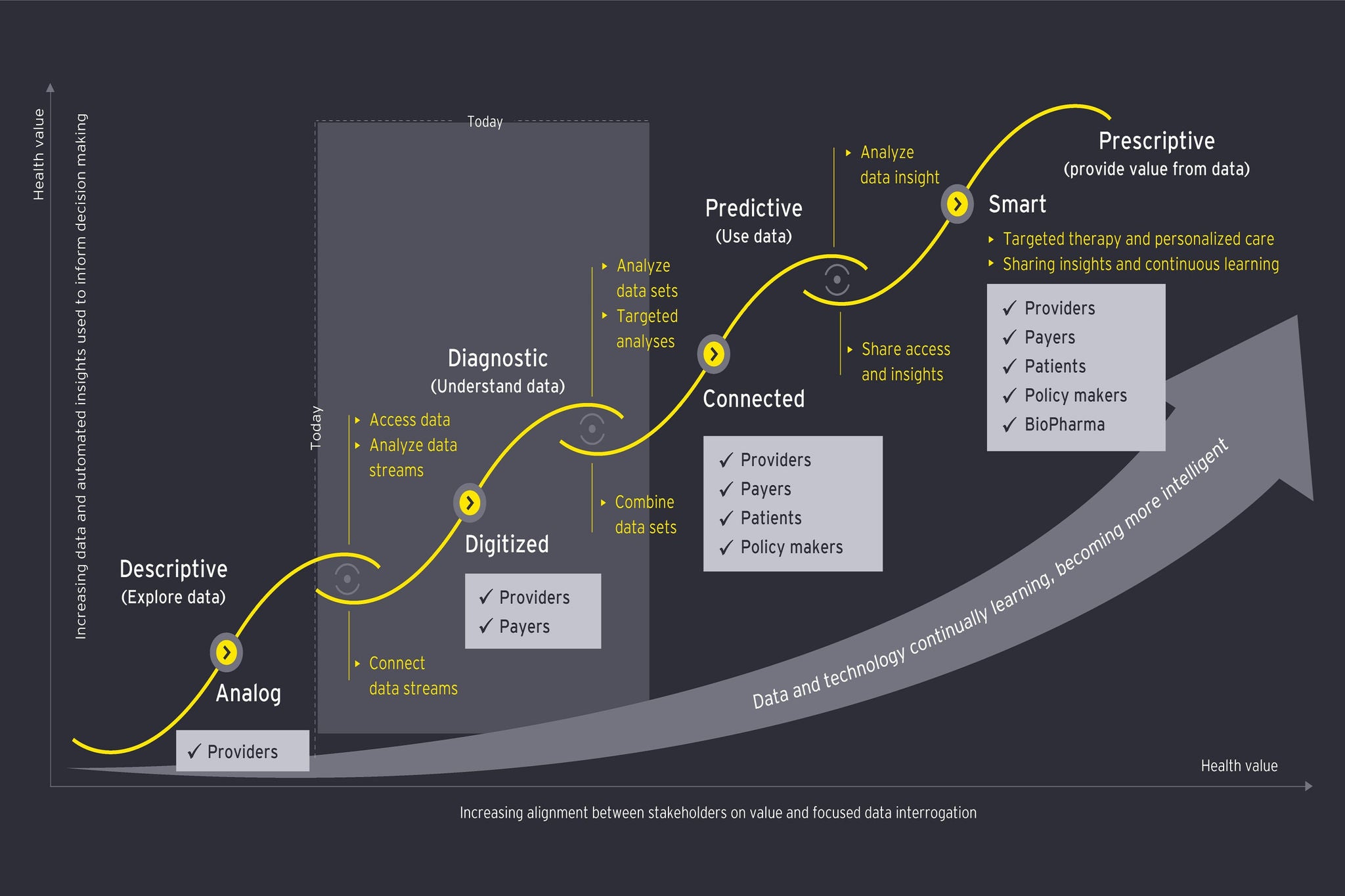
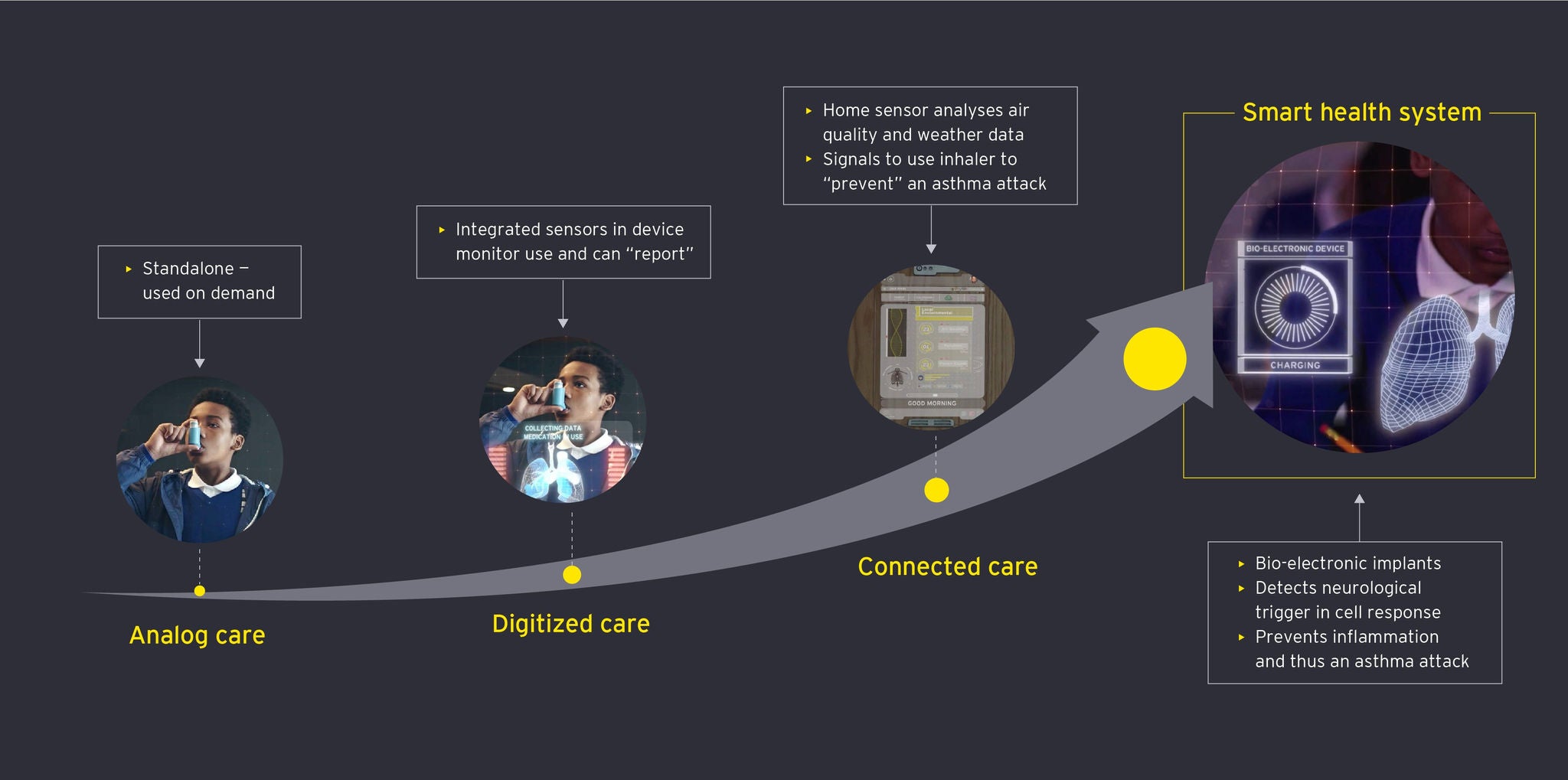
Similarly, the “smart implants” of today will become just one node in a digital ecosystem delivering post-operative care. While today’s patients are discharged home to manage their own recovery and self-care with limited guidance or contact, the patient in the near future will access home coaching via digital personal assistants. Linked to the data from their smart implant, which will help optimize the coaching program, the patient will experience a guided and accelerated path through rehabilitation. Further on, the post-operative patient in the IHE will receive still more personalized and effective management. A simulated digital twin built from rich data from the implant and the smart home environment will enable personalized, interactive physio sessions modelled around the patient’s individual needs.
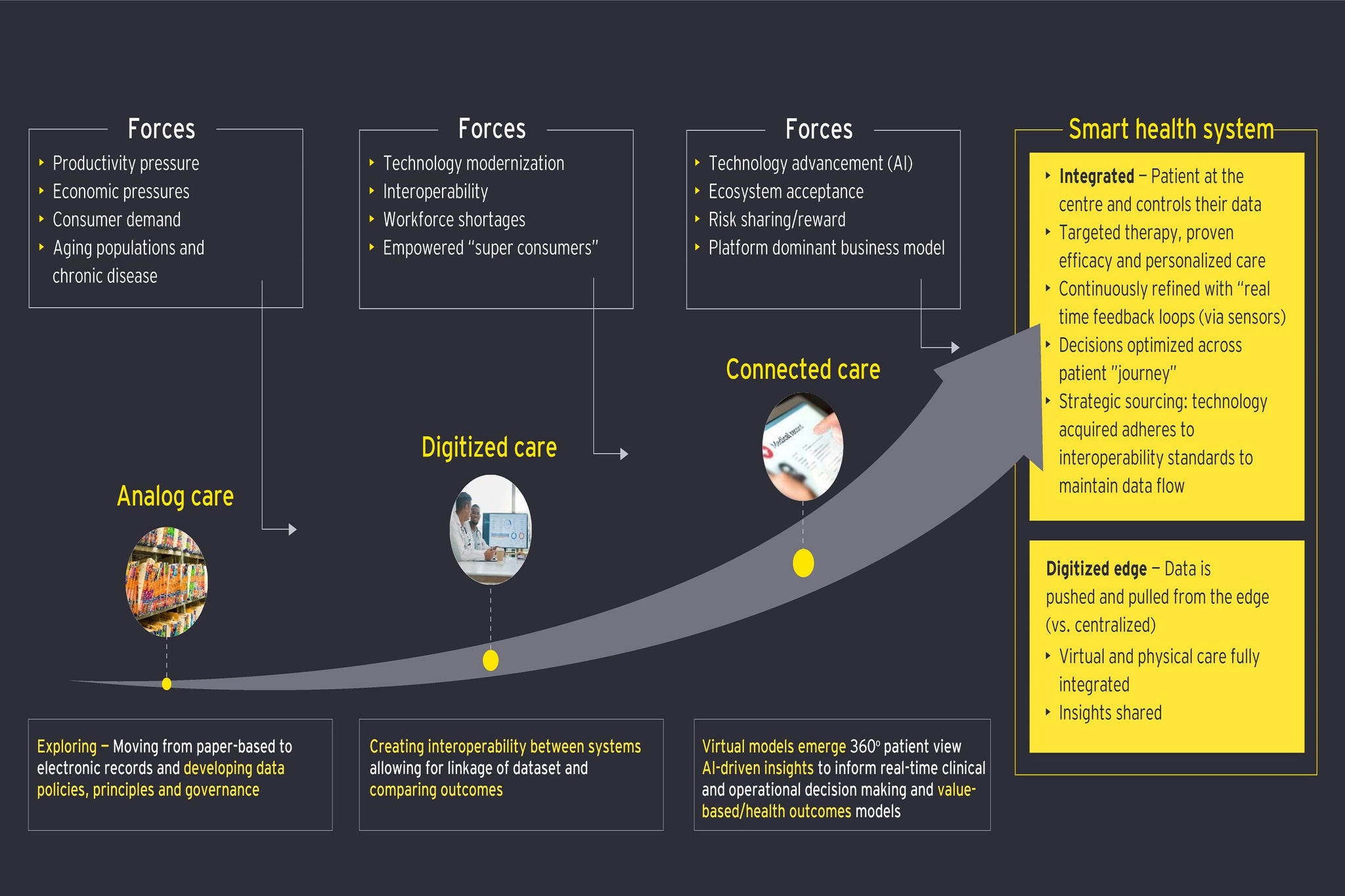
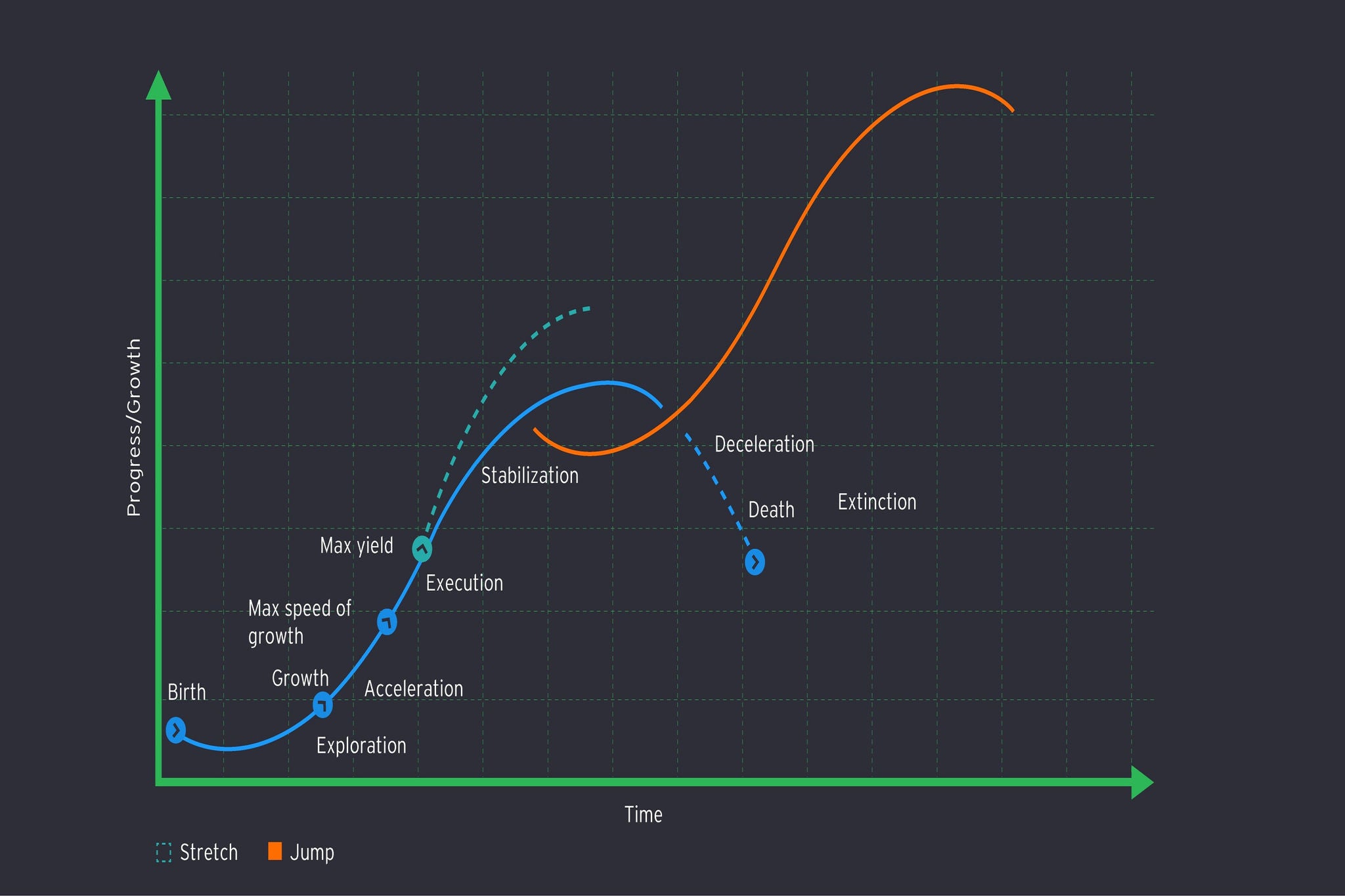
Instead of care being dispensed at brick-and-mortar sites the patient visits only sporadically, we can envisage at the end of the journey through digitized and connected care to the IHE a world where health management has effectively become ambient, technology surrounding the patient in a moving cloud of care that constantly optimizes itself for better outcomes. Where today we have some digital telehealth additions to our legacy systems, the future will see the increased presence of virtual hospitals offering comprehensive specialist support, remote yet highly personalized and even predictive. As the IHE evolves, we will go further yet, and see the emergence of large-scale specialized remote care, where medical engineers effectively manage huge numbers of patients at a distance through data and technology.
This new approach to care will deliver the outcomes each stakeholder seeks. Providers will have the information and the tools to deliver care far more effectively than can be achieved today. Payers and policymakers will be investing their resources in care that genuinely works. Smarter care will save patients the need for long and costly hospital visits, maintain the wellbeing and productivity of the population and enable policymakers to see health care (which today could more accurately be described as “sick care”) not simply as a financial burden but as a public asset to society. The organizations that enable these more effective new care approaches will also be appropriately valued for the benefits they have delivered. Differential reimbursement within the VBC system will reward and sustain innovation.
The better personalized health experience the IHE will deliver is not a luxury but a necessity
VBC will streamline operating models and introduce both efficiency and efficacy through the ability to personalize treatments. At present much health spending is mis-directed and wasted because we have too little data to predict what interventions will help which patients. Most of all, this progress towards the IHE will transform for the better the individual patient’s experience and outcomes. Personalization of care is not a luxury but an essential step in widening access and health equity.
The industry and its stakeholders have for too long underestimated how important the quality of health experience is for patients. In other industries, market leaders have shown the importance of convenience, choice, seamless transactions, transparency, and personalization in delivering a better user experience. Health care has been slow to learn these lessons; but as our care systems become more digitized, connected, and smart, improving health experience will become a key concern. In the past the individual’s subjective experience has been seen as a marginal concern, with clinical results the focus. Yet experience is central to delivering better outcomes: engaged, empowered patients are not simply happier, but also healthier.
The IHE offers a health care future that can meet the needs of the industry, its stakeholders and the patients they collectively serve. The technologies to realize that vision are here now. The organizations that can realize the long-term effects of these technologies to exponentially change the way we deliver health care will be the leaders in this new era. They will secure their position at the heart of the emerging ecosystem that will deliver health care fit for the future.