EY refers to the global organization, and may refer to one or more, of the member firms of Ernst & Young Global Limited, each of which is a separate legal entity. Ernst & Young Global Limited, a UK company limited by guarantee, does not provide services to clients.

Our latest report spotlights four focus areas where Nordic health organizations can improve access, experience and outcomes.
In brief
- Interviews with global health executives reveal inadequate analytics stalls many efforts to extract actionable data insights around mental health.
- Health executives want to see more consistency in the practice of mental health care and a focus shift of dollars from acute care to prevention.
- Digital health transformation holds the key to improved mental health care by providing better data insights and fostering an integrated care ecosystem.
According to our latest Global Consumer Health Survey 2025, nearly half of the respondents (49%) rated the mental health care system in their country as fair or poor. However, they expressed significant openness to preventive mental health screenings, with eight in 10 indicating they would be willing to undergo an annual mental health check-up if it were available at no or minimal cost.
Access remains an issue, with 46% citing long wait times as a barrier to care. In some interviews, health executives shared their own battles in getting proper mental health care for their loved ones. “I can't believe the number of calls I get from people, even strangers, who say my daughter or son is really struggling,” said one health executive in an interview with the EY organization.
Across the globe, long wait times too often lead to deteriorating symptoms that present as crisis cases in the emergency room. In the Nordics, experts interviewed also cited shortages of psychiatrists and specialty psychologists as contributing to the challenges.
The new research spotlights a path forward to deliver better outcomes and experiences via a system that demystifies the journey, is more transparent about costs and outcomes and helps connect people to the right providers at the optimal time throughout their care. Nearly all of the health care experts interviewed said better data insights are critical to help countries understand the mental health needs of the population and of individuals, so they can intervene more effectively and drive toward more measurement-based care.
Watch our latest webinar on Transforming care models for improved mental health care
Impatient stakeholders aren’t seeing the value
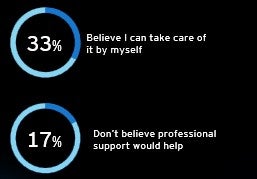
However, health care systems have not convinced health care consumers of the value of mental health care delivery. One in three (33%) respondents to the survey said they can take care of the problem themselves while another 17% said professional help doesn’t work.
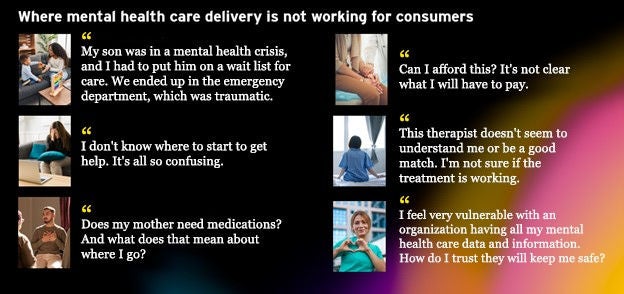
The skepticism could be attributed to the journey itself, as consumers indicate they are confused about the system. More than one-third said they were either unsure of how to find support or found the information about mental health difficult to understand. Our findings show consumers are challenged by access, cultural barriers and not understanding what type of care they need, whether it be a psychologist who can provide talk therapy, a psychiatrist who can prescribe medication, a peer counselor or someone in between. Financial reasons and lack of transparency about costs also are a major concern.
The solution lies in digital health transformation
1. Improve mental health data analytics for better and more equitable outcomes
To improve health organizations’ ability to have a true sense of their population’s needs, better data insights are needed to enable teams to proactively intervene on an individual level.
Sølve Braut, head of the psychiatric department at Stavanger University Hospital, said there is access to extensive data. “But more analytical capacity is needed rather than more data,” he said.
The proper data infrastructure is also critical for applying basic analytics or artificial intelligence (AI) tools to gather insights on patient demand and needs. As health systems try to build this infrastructure, they should be guided by governance policies that acknowledge the unique data privacy regulations over health and mental health data and determine how to use the data in ways that ensure trust. When integrating systems and applying AI, that governance will be important to avoid the introduction of bias or hallucinations that could exacerbate already existing challenges.
The survey also found that global consumers are open to digital tools that can help with mental health, as long as health organizations are transparent and help them see the value of using digital health technologies to connect them with providers, peer groups and other supports. Sixty percent of respondents said they would feel comfortable using genetic tests that show whether they are predisposed to have certain mental health conditions; 59% would feel comfortable using digital technologies that collect and share their mental health data with providers. Health organizations need to embed privacy and security in their design of all infrastructure, apps and algorithms. Patients want to know their data is encrypted end-to-end and that it will not leave the systems they have approved to access their data.
2. Transform care models for better triage, more prevention and integration
Interviews and survey results highlight the barriers to accessing timely mental health care and these barriers can result in inefficiency and waste. When people are not routed appropriately, too many progress to a crisis situation, focusing the system resources on inpatient beds and acute care. Meanwhile, issues that could be resolved earlier with less suffering, cost and burden to the system go unaddressed.
Health leaders also voiced a desire for more standardization in the delivery of mental health care, such as has been done clinically with creating pathways for conditions such as high blood pressure and diabetes.
Interviews highlight the ability of integrated mental health care teams to provide the right level of care when consumers need it, adjusting care as necessary, especially when many who are struggling do not know what they need. Across the globe, health systems have turned to different integrated models, from those focused on bringing primary care, behavioral health, sexual health and other providers together under one roof to peer-group led cafes. Braut pointed out that integration remains complicated in Norway because of the division of responsibilities between municipalities and specialist health services.
The survey suggests that health care providers can be an entry point to the mental health care system, with 61% of consumers already seeking help from their primary health care provider for mental health concerns. Nearly 70% of respondents said they were very or somewhat comfortable addressing mental health care with their primary care doctor, with older generations being more likely to both have a doctor and be comfortable with them. But taking advantage of this opportunity would require integrated data platforms and a more coordinated ecosystem focused on prevention.
Payers and governments have a role to play in incentivizing a shift to more preventive, predictive, affordable mental health care that provides consistency in care quality. “Eventually what drives innovation is reimbursement. As long as insurance companies are not picking up on the roadblocks, we will not be moving forward,” said Luisa Wasilewski, founder of Berlin-Germany based Pulsewave Digital. “It is the regulators that change the system, not technology.”
Another digital avenue for health organizations to pursue is to build intuitive, helpful digital front doors through online portals or apps that improve the mental health care experience, connecting consumers to care when they need it.
3. Show value and progress to consumers, payers and stakeholders
More than half of global survey respondents (55%) report that financial or insurance issues have caused them to stop or consider stopping the use of professional mental health services. If they are already concerned about affordability and not convinced of the value, health organizations could make gains by educating consumers and other stakeholders about the value of mental health care, helping them understand treatment decisions and how realistic progress looks.
Kirsten Horthe, Head of Psychiatric Unit, Vestre Viken Hospital Trust in Norway, highlighted how her organization uses technology to help patients understand their progress. Through a program called “Share with Me,” the team deployed a form that each patient receives before treatment and during treatment that provides consistent feedback on progress. “If the patient actually feels that there is no progress here, then it is given back to the therapist,” she said. “It's a way we use technology in a smart way, to slowly get better at systematizing the feedback. If not, then it is a closed room - the therapy room. If things go badly, then it is not certain that the therapist is doing the right things. If you get warning signals through these forms that it is suicidality then that escalates, then you also get the opportunity to intervene earlier.”
The lack of measurement-based care hampers the ability of providers to make the case to consumers and payers that mental health care services are valuable. And other stakeholders point to a lack of accountability when it comes to delivering quality mental health outcomes.
4. Invest in the areas where consumers say health organizations are failing in important ways
The EY organization’s consumer research highlights the key moments in mental health journeys where health organizations can significantly improve interactions that consumers find both important and challenging.
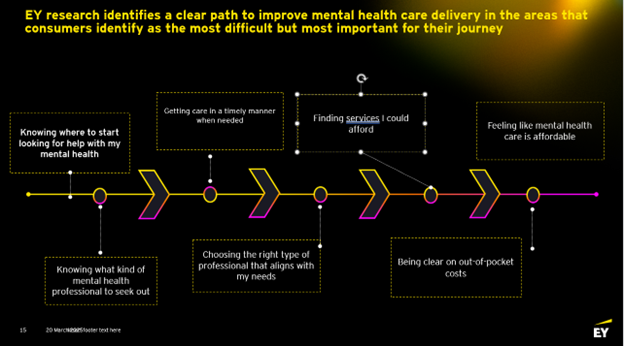
A third of global respondents (32%) cited a lack of mental health professionals with skills specific to their needs; 50% of those who have used mental health services changed their mental health professional, with the top reasons cited as lack of personal connection or compatibility (42%) or not satisfied with progress (37%). The survey suggests consumers are overwhelmed with information and don’t know what type of provider they need. They struggle to access care in a timely fashion and to understand their financial costs, leading to inequities.
Key takeaways
By age 75, half the global population is expected to develop one or more mental disorders during their lifetime. Countries around the globe have declared crises as their youth and adult populations struggled with increased rates of depression, loneliness, anxiety and other challenges.
The lack of investment worldwide in preventive mental health care does not mean society is escaping these costs. Anyone who has waited with a child or loved one in a mental health crisis knows how terrifying it can be and how confusing it can be to know where to go, who to trust, what kind of help is needed, what it will cost and whether it will work. Post-COVID-19 pandemic, the costs to society, to families, to providers and health systems are evident. More effective, transparent, preventive and affordable mental health care journeys are the way forward.
Summary
The article highlights four key areas for Nordic health organizations to improve mental health care delivery. It reveals that inadequate analytics hinder actionable insights, while health executives advocate for a shift from acute care to prevention. The research emphasizes the need for improved data analytics, standardized care models and effective communication of mental health care value to consumers and stakeholders. Ultimately, a focus on transparency, prevention and integration is vital for enhancing mental health care outcomes.
