Given these types of disruptive trends, profitability initiatives may prove more complex and slower to implement than working capital improvements. A powerful way for hospitals to address these challenges is to free up liquidity through better cash management techniques. Effective cash management is essential for maintaining financial health, enabling investments in technology and infrastructure, and ensuring long-term sustainability.
Net working capital (NWC) represents an area with untapped potential. A recent EY-Parthenon analysis indicated that NWC among hospital systems ranges greatly, from 5% to 20% of total revenues, with some organizations exceeding 25%. Over the past five to seven years, there has been a steady trend of 1% to 3% annual increases in NWC among these systems. Private healthcare institutions often exhibit even greater disparities, with estimates suggesting that over 30% of total revenues may be tied up due to higher operational costs, delayed reimbursements, and the need for substantial investments in technology and infrastructure. While optimal NWC targets vary by organizational size, type and location, the healthiest of systems have less than 10% of their total revenue tied to NWC and have clear visibility of cash inflows and outflows.
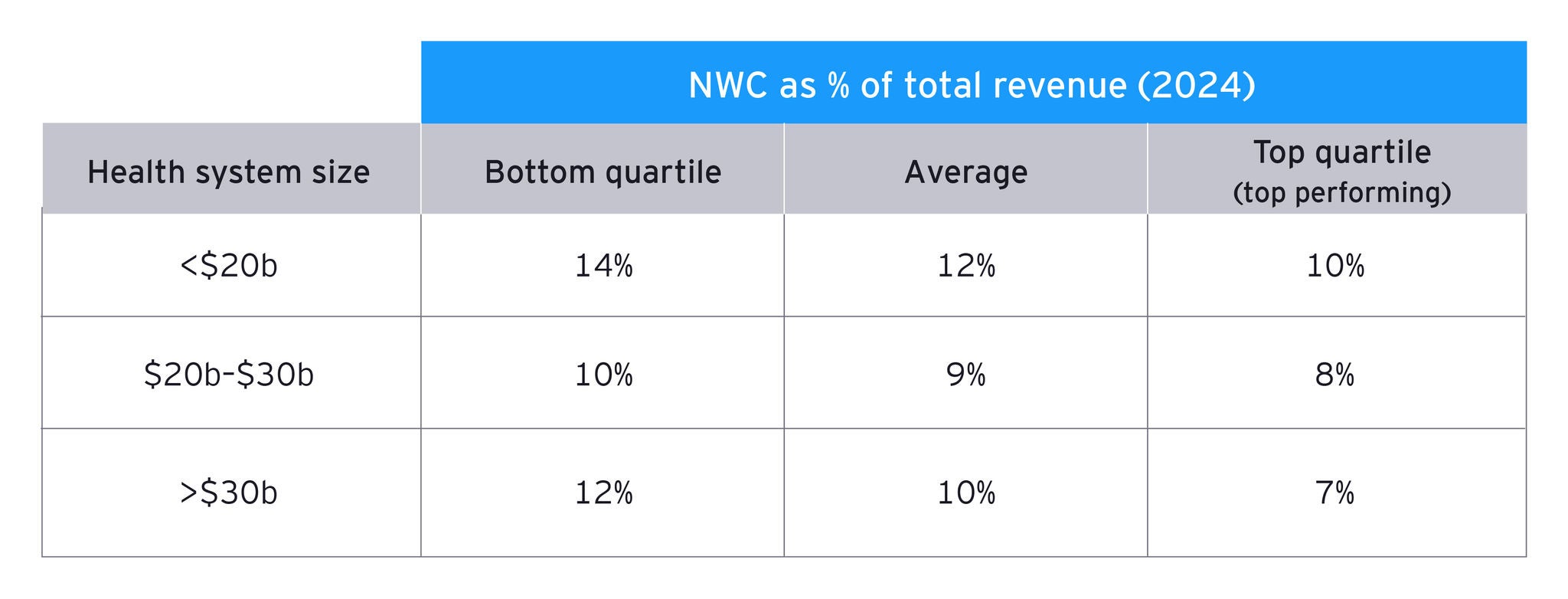
The following table (Figure 1) depicts the top public hospital systems and their NWC as a percentage of total revenue. The top performers, on average, are 1%–3% better than the average hospital system, equating to freeing up $500 million to $1 billion of cash tied up in working capital.
Figure 1: Net working capital as % of total revenue - 2024 view